New Treatment for Adults with Acute Lymphoblastic Leukemia Approved by the FDA
This week’s excitement surrounding the groundbreaking U.S. Food and Drug Administration (FDA) approval of the CAR T–cell therapy tisagenlecleucel (Kymriah) for treating certain pediatric and young adult patients with acute lymphoblastic leukemia (ALL) was not the only good news for ALL community in August. Earlier in the month, the FDA approved a new molecularly targeted therapeutic called inotuzumab ozogamicin (Besponsa) for treating adults who have B-cell precursor ALL that did not respond to initial treatment or that returned after treatment.
ALL is more commonly diagnosed in children and adolescents (those age 19 and younger) than in adults (those age 20 and older), according to data from the National Cancer Institute Surveillance, Epidemiology, and End Results Program. Substantial progress has been made in the treatment of pediatric ALL; the five-year relative survival rate among those ages 0 to 14 at diagnosis is 90 percent. However, the prognosis for adults diagnosed with ALL is not as good, with five-year survival rates estimated to be around 30 percent to 40 percent.
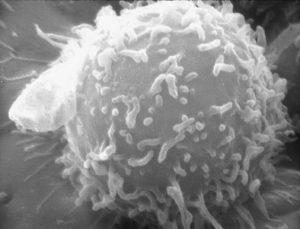
About 75 percent of adults with ALL are classified as having B-cell ALL, which means their leukemia originated in immune cells called B cells. Most B-cell ALL cells have a protein called CD22 on their surface, making it an attractive therapeutic target.
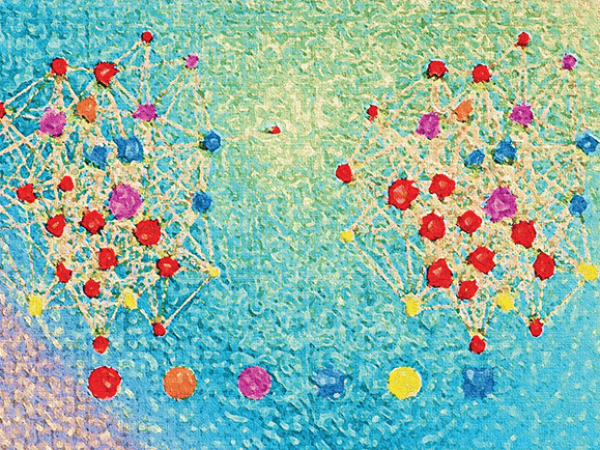
Inotuzumab ozogamicin is a type of molecularly targeted therapeutic known as an antibody-drug conjugate. These therapeutics use an antibody to deliver an attached cytotoxic agent directly to those cancer cells that display the antibody’s target on their surfaces. The precision of antibody targeting reduces the side effects of the cytotoxic agent compared with traditional systemic delivery. In the case of inotuzumab ozogamicin, the cytotoxic agent calicheamicin is attached to a CD22-targeted antibody using a linker. When the antibody attaches to CD22 on the surface of B-cell ALL cells, the antibody-drug conjugate is internalized by the leukemia cells. This leads to calicheamicin being released from the linker and antibody. Once free, calicheamicin causes DNA damage, which ultimately triggers the leukemia cell to die.
The approval of inotuzumab ozogamicin was based on results from the phase III INO-VATE ALL clinical trial, which were published in The New England Journal of Medicine. These data showed that the rate of complete remission for those who received inotuzumab ozogamicin was more than double the rate for those who received standard chemotherapy. The number of patients who were able to go on and have a stem-cell transplantation was also more than double among those treated with inotuzumab ozogamicin than among those in the standard-therapy group. Stem-cell transplantation is the only potentially curative treatment option for patients whose ALL does not respond to, or relapses after, initial treatment.
In addition, progression-free and overall survival were improved among those receiving inotuzumab ozogamicin, although the improvement in overall survival did not meet the pre-specified boundary for statistical significance.
It is important to note, however, that there were several severe adverse events reported in the INO-VATE ALL trial. These raised sufficient concern at the FDA that the approval comes with a boxed warning indicating that inotuzumab ozogamicin can cause liver toxicity and increase risk of death following certain types of stem-cell transplant and suggesting that patients being treated with inotuzumab ozogamicin need to be monitored closely by their health care providers.