Putting the Brakes on Triple-negative Breast Cancer
Breast cancer is the most common cancer among women in the United States and worldwide, with an estimated 2.1 million women diagnosed each year. While incredible strides have been made over the past few decades in reducing the death toll from this disease, breast cancer still accounts for approximately 15 percent of all cancer-related deaths in women.
The disease is particularly devastating for women diagnosed with a form of breast cancer known as triple-negative breast cancer (TNBC), so named due to the absence of three receptors on the cell surface. The poor prognosis of TNBC, relative to other breast cancer subtypes, is largely due to the paucity of treatments available for this subtype.
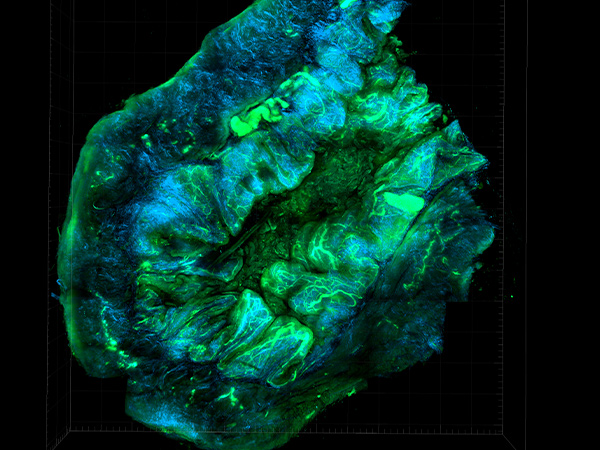
In recent years, immune checkpoint inhibition has been explored as a potential treatment option for TNBC. This form of immunotherapy keeps immune cells active by preventing PD-L1, a protein on cancer cells, from engaging the PD-1 receptor on immune cells, thereby releasing the “brakes” on the immune system and allowing it to destroy the cancer. TNBC may be well suited for treatment with immune checkpoint inhibitors because it has high levels of immune-promoting cells called tumor-infiltrating lymphocytes, which have been shown to correlate with responses to immune checkpoint inhibition, and because TNBC cells express high levels of PD-L1.
Immune checkpoint inhibition is benefiting some patients with TNBC, including survivor Eva Joseph, whose story was featured in the AACR Cancer Progress Report. Joseph was diagnosed with stage 4 TNBC in 2014 after metastatic tumors were discovered in her sternum and lungs. She enrolled in a clinical trial testing the immune checkpoint inhibitor atezolizumab (Tecentriq), which targets PD-L1, in combination with the chemotherapy nab-paclitaxel (Abraxane), which led to a reduction in the size of her tumors. Six years after she began receiving treatment, Joseph’s cancer remains at bay. In 2019, atezolizumab plus nab-paclitaxel, the combination treatment she received, was approved by the U.S. Food and Drug Administration (FDA) for the treatment of some patients with locally advanced or metastatic TNBC.
Last week, the FDA approved another immune checkpoint inhibitor, the PD-1 inhibitor pembrolizumab (Keytruda), in combination with chemotherapy for the treatment of patients with locally recurrent unresectable or metastatic TNBC. The approval was based on results from the KEYNOTE-355 clinical trial showing that patients treated with pembrolizumab in combination with chemotherapy had greater progression-free survival than patients who received placebo plus chemotherapy. These results will be presented at the upcoming San Antonio Breast Cancer Symposium (SABCS), which will be held December 8-11 and is co-sponsored by the AACR, UT Health San Antonio, and Baylor College of Medicine.
Clinical trials continue to explore additional immune checkpoint inhibitor regimens for TNBC, including for the treatment of early-stage disease. Last year’s SABCS and the 2020 AACR Virtual Annual Meeting I featured results from some of these studies.
KEYNOTE-522
One of the clinical trials presented at SABCS 2019 was the KEYNOTE-522 trial, which is evaluating pembrolizumab in combination with neoadjuvant chemotherapy and as adjuvant therapy in patients with previously untreated, early-stage TNBC. Patients were treated with either pembrolizumab plus chemotherapy or placebo plus chemotherapy as neoadjuvant treatment. After surgery, patients received either adjuvant pembrolizumab or placebo until recurrence or unacceptable toxicity.
The rates of pathologic complete response (pCR)—which is the complete absence of cancer after neoadjuvant treatment—were reported at the meeting. Patients with TNBC who have a pCR after neoadjuvant therapy tend to have a more favorable outlook. At the time of analysis, patients in the pembrolizumab plus chemotherapy arm had a significantly higher rate of pCR compared to patients in the chemotherapy-alone arm (64.8 percent vs. 51.2 percent).
The researchers also examined pCR rates in patients whose cancers had spread to the lymph nodes, since lymph node involvement is associated with a higher risk of TNBC recurrence. Among these patients, 64.8 percent of those in the pembrolizumab plus chemotherapy arm had a pCR, compared to 44.1 percent in the chemotherapy-only arm.
“Our results suggest that adding pembrolizumab to neoadjuvant chemotherapy is beneficial for patients with the most aggressive disease and the highest unmet need,” said researcher Peter Schmid, MD, PhD, in an AACR press release. “I think the results have the potential to be practice-changing.”
NeoTRIPaPDL1
Another study presented at SABCS 2019 was the NeoTRIPaPDL1 trial, which is evaluating atezolizumab with chemotherapy in the neoadjuvant setting for patients with early or locally advanced TNBC. This is the same immune checkpoint inhibitor that was approved for locally advanced or metastatic TNBC in 2019.
In the NeoTRIPaPDL1 trial, patients were randomly assigned to receive neoadjuvant atezolizumab plus chemotherapy or neoadjuvant chemotherapy alone. Last December, when results were presented at SABCS, the researchers had not observed any statistically significant differences in the rates of pCR between the patients who received atezolizumab and those who did not.
“Our observations may indicate that there is no therapeutic benefit to adding atezolizumab to neoadjuvant chemotherapy compared to chemotherapy alone, or it may simply mean that any beneficial effects of the combination will be seen in the long term,” researcher Luca Gianni, MD, explained last year in an AACR press release.
Updated results presented at the 2020 ESMO Virtual Congress in September shed some light on these findings. The latest results showed that patients in the chemotherapy-only arm had higher baseline levels of tumor-infiltrating lymphocytes compared with those in the atezolizumab plus chemotherapy arm. Since the presence of these immune cells would be expected to improve responses, this discrepancy may help explain the similarity in pCR rates between the two treatment arms.
The updated results also revealed that while there were no significant differences in overall pCR rates between the two arms, there were significant differences between the treatment arms among patients who were defined as “immune-rich” based on PD-L1 expression or on the presence of tumor-infiltrating lymphocytes in the stroma or within the tumor itself. Among immune-rich patients, pCR rates were significantly greater for those treated with neoadjuvant atezolizumab plus chemotherapy compared with those receiving neoadjuvant chemotherapy alone (86.9 percent vs. 72.0 percent).
These results suggest that adding atezolizumab to neoadjuvant chemotherapy may improve pCR rates in a subpopulation of patients with early or locally advanced TNBC.
I-SPY 2
The 2020 AACR Virtual Annual Meeting I featured results from an arm of the I-SPY 2 clinical trial, which, among other queries, is evaluating the impact of adding the immune checkpoint inhibitor durvalumab (Imfinzi), which targets PD-1, and the targeted therapy olaparib (Lynparza) to neoadjuvant chemotherapy in patients with breast cancer, including 21 patients with TNBC.
Of the patients with TNBC, a pCR was seen in 47 percent of those treated with neoadjuvant durvalumab, olaparib, and chemotherapy, as compared with 27 percent of those treated with neoadjuvant chemotherapy alone. Additional research will be required to determine whether the improved responses were due to durvalumab, olaparib, or both.
TONIC
The TONIC trial is a phase II clinical trial evaluating the PD-1 inhibitor nivolumab (Opdivo) after treatment with either chemotherapy or radiation therapy in patients with metastatic TNBC. Researchers are interested in understanding whether short-term pretreatment with chemotherapy or radiation therapy could improve responses to nivolumab; such pretreatment is referred to as “induction therapy.” The trial includes 67 patients with metastatic TNBC who were randomly assigned to receive nivolumab without induction therapy, or after induction with radiation or one of three chemotherapeutics (cyclophosphamide, cisplatin, or doxorubicin).
Interim results published last year showed that the overall response rate was greatest for patients who received induction therapy with doxorubicin (35 percent), followed by cisplatin (23 percent), no induction (17 percent), cyclophosphamide (8 percent), and irradiation (8 percent). These findings suggest that induction with doxorubicin or cisplatin is feasible and could improve responses to nivolumab in patients with TNBC, but further investigation will be required to understand the factors influencing the observed response rates.
JAVELIN
The phase I JAVELIN study, which concluded in December 2019, examined the safety and efficacy of the PD-L1 inhibitor avelumab (Bavencio) for patients with various solid tumors. The study enrolled 168 patients with pretreated metastatic breast cancer, including 58 patients diagnosed with metastatic TNBC. Results published in 2018 showed that the overall response rate to avelumab for patients with metastatic TNBC was 5.2 percent, with patients whose cancers expressed PD-L1 having a higher overall response rate than those whose cancers were PD-L1-negative (22.2 percent vs. 2.6 percent). Grade 3 or higher adverse events were observed in 13.7 percent of patients, and there were two treatment-related deaths. The authors concluded that avelumab has an acceptable safety profile and may have clinical activity in patients with metastatic TNBC, particularly those with PD-L1-positive cancer.
While patients diagnosed with TNBC often face a poor prognosis, the advent of immune checkpoint inhibition offers a gleam of hope. Each of the clinical trials described here is examining a different immune checkpoint inhibitor under a unique disease and treatment context, representing just a few of the diverse approaches being explored to treat TNBC. Clinical trials such as these provide valuable information that can ultimately guide future research, transform treatment paradigms, and improve outcomes.
A complete list of the ongoing clinical trials that are evaluating immune checkpoint inhibitors for TNBC can be found here.



Sadly we are facing the illness of the century. Cancer is a very aggressive and destructive enemy of our bodies.