AACR Annual Meeting 2021: AACR Project GENIE Powers Research on Cancer Disparities and Clinical Outcomes
The term “cancer” encompasses a broad range of diseases that can afflict almost any organ of the body. Not only do molecular features and clinical outcomes vary widely between different cancer types, but they can even differ between individuals who have the same cancer. Given this vast heterogeneity, how do physicians select the appropriate treatment course for each patient?
Precision medicine is a growing field of cancer medicine that aims to tailor a patient’s treatment to the unique features of their own tumor. Early versions of this approach, including therapies that target mutated versions of HER2, BRAF, or MEK, among others, have shown success for some cancers. Now, researchers are analyzing the genetic features of patient tumors to identify additional targets and to understand the factors that might influence clinical outcomes in diverse diseases and patient populations.
While advances in next-generation sequencing have helped push precision medicine forward, several challenges remain. The limited data available for rare cancer types, genetic variants, and/or patient subsets has made certain diseases and populations difficult to study. Furthermore, many existing genetic databases typically only include data from patients enrolled in clinical trials and from a specified period of time.
To address these limitations, AACR Project GENIE (for Genomics Evidence Neoplasia Information Exchange) was launched in 2015 with the goal of improving clinical decision-making by linking genotype to outcomes, according to Philippe Bedard, MD, chair of the AACR Project GENIE Steering and Education Committees. Speaking during a session of the AACR Annual Meeting 2021, Bedard explained that Project GENIE is an international pan-cancer registry of real-world data enabled by data-sharing. The latest release includes data from 19 leading cancer centers.
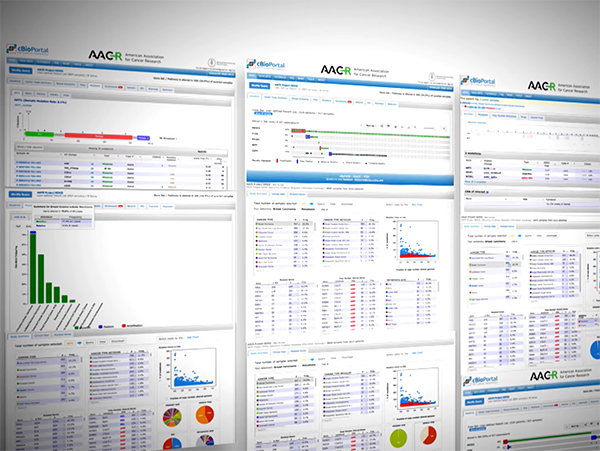
Unlike some other genetic databases, Project GENIE includes genomic and clinical data from patients undergoing routine oncology care, rather than focusing only on clinical trial participants. Moreover, the database is updated as additional data from these patients is gathered over time, allowing researchers to study the natural course of disease. Due to the collection of data from cancer institutions around the world, Project GENIE enables research into rare disease types and patient populations in a way that would not be possible with the small sample sizes at a single institution.
The power of Project GENIE to uncover genetic determinants of cancer risk and clinical outcomes was illustrated during a session of the Annual Meeting titled “Advancing Cancer Research Through An International Cancer Registry: AACR Project GENIE Use Cases.”
Uncovering genetic differences by race in early-onset colorectal cancer
Two studies presented during this session used Project GENIE data to define genetic features of early-onset colorectal cancer (CRC) by race. Approximately 10 percent of CRCs are early-onset, meaning they are diagnosed in patients under 50 years of age, explained Andreana Holowatyj, PhD, MS, an assistant professor of medicine and cancer biology at the Vanderbilt University Medical Center and Vanderbilt-Ingram Cancer Center. The incidence of early-onset CRC has been steadily increasing over the past 25 years, and certain racial/ethnic groups suffer from higher incidence and mortality rates.
Holowatyj and colleagues examined the genetic features of early-onset and late-onset CRC by self-reported race. “The unique…information found within the AACR Project GENIE database…provided us with sufficient cases to study this disease across diverse populations in a way that we would not be able to at individual institutions,” Holowatyj noted in an AACR news release on this study.
Holowatyj’s study was also featured in a video on AACR Stories, the Faces and Voices Behind the Science, and in a news article in the AACR journal Cancer Discovery.
According to the results presented by Holowatyj, Black patients with early-onset CRC had significantly higher tumor mutational burden compared with non-Hispanic white patients. Since tumor mutational burden is a biomarker that may predict responses to certain cancer therapies, the observed differences between races could have implications for cancer treatment.
The researchers also compared the mutations of early-onset CRCs with late-onset CRCs within each racial group, which uncovered race-specific differences between early- and late-onset tumors. Among non-Hispanic white patients, early-onset CRCs were more likely to have mutations in the LRP1B, TP53, TCF7L2, DOCK8, SMAD2, and SMAD3 genes compared with late-onset CRCs, and less likely to have KDR and FLT4 mutations. However, early-onset CRCs from Black patients were more likely to have mutations in CREBBP and TGFBR2 when compared with late-onset CRCs from Black patients. Tumors from Asian/Pacific Islander patients with early-onset CRC were less likely to present with mutations in APC and PIK3CA, and were more likely to have mutations in FAT1 compared with those of Asian/Pacific Islander patients with late-onset CRC.
“This study provides first-of-its-kind evidence that molecular features of early-onset CRC may differ by race,” Holowatyj concluded. “The development of therapeutic modalities that target these distinct molecular features may yield clinical implications for early-onset CRC.”
Holowatyj added that “race is a social construct and [only] one piece of the puzzle. Trying to address this complex interrelated network of factors that could be contributing to the biology underpinning disparities…is also a direction moving forward that’s important to consider.”
David Hein, a research assistant at University of Texas Southwestern (UTSW) Medical Center, and colleagues also utilized data from Project GENIE, in conjunction with data from UTSW, to explore the genetic features of early-onset CRC by race/ethnicity. The analysis focused on 22 genes that are commonly mutated and have clinical implications in CRC, including genes involved in cell signaling, tumor suppression, and DNA repair. Hein and colleagues also analyzed copy number variations in ERBB2, MET, EGFR, and SMAD4.
Mutations in four genes were found to be significantly enriched in early-onset CRCs by race/ethnicity: Mutations in the KRAS signaling gene were enriched among non-Hispanic Black patients, mutations of the tumor suppressor APC were enriched among non-Hispanic white patients, and mutations in the DNA repair gene PMS2 and the signaling gene NTRK2 were enriched among Hispanic white patients.
Since KRAS mutations are predictive of poor response to EGFR-targeted therapy, it is “possible that increased KRAS mutations could contribute to worse prognosis in early-onset CRC in Black patients,” Hein noted, though additional research will be required to test this hypothesis.
In addition to the enrichment of PMS2 mutations in white Hispanic patients, five other DNA repair genes (MLH1, MSH2, MSH6, BRCA1, BRCA2) were also more commonly mutated in early-onset tumors from white Hispanic patients compared with other racial/ethnic groups. However, the higher mutation rates of these five DNA repair genes were not statistically significant. No significant differences by race/ethnicity were observed for copy number variations of ERBB2, MET, EGFR, or SMAD4.
“Differences in clinical outcome may be explained by differences in genomic features,” suggested Hein. “Our findings highlight the need for more effort in ensuring diversity in genetic databases so that we are adequately representing our diverse young CRC population.”
Examining treatment outcomes in non-small cell lung cancer
A tumor’s genetic features can impact how it responds to treatments. To define how various molecular subtypes of non-small cell lung cancer (NSCLC) respond to different therapies, two studies examined clinical outcomes from private datasets within Project GENIE that are scheduled for public release later this year.
Beilei Cai, PhD, a senior director at Novartis Pharmaceuticals, presented data on treatment outcomes for NSCLCs with wild-type (wt) EGFR and ALK. While NSCLCs that have EGFR mutation or ALK rearrangement can be treated with EGFR- or ALK-targeted therapies, respectively, patients whose NSCLCs do not have either of these molecular features are ineligible for such therapies.
In this study, Cai and colleagues examined survival data of 263 patients with wtEGFR/wtALK advanced NSCLC who received first-line treatment with chemotherapy, immunotherapy, targeted therapy, or a combination of bevacizumab and chemotherapy. All patients were treated between 2014 and 2017 and had undergone next-generation tumor sequencing within 60 days of treatment initiation. Among patients with stage 4 NSCLC, median progression-free survival was 4.2, 4, 6.2, and 6.8 months for those treated with chemotherapy, immunotherapy, targeted therapy, and bevacizumab plus chemotherapy, respectively. Median overall survival was 19.7, 18.4, and 23.5 months for patients with stage 3/4 disease who received chemotherapy, immunotherapy, and bevacizumab plus chemotherapy, respectively. The median overall survival was not reached for patients receiving targeted therapy. Due to the descriptive nature of the analysis, Cai cautioned against making direct comparisons between survival outcomes of the different treatment groups.
“This study is the first reported analysis of real-world data for advanced NSCLC using the AACR [Project] GENIE database,” said Cai, adding that follow-up analyses will be prudent to account for recent treatment developments. “Although those without EGFR or ALK mutations may still have treatment options, such as immunotherapy, chemotherapy, or targeted therapy, there are still high unmet medical needs.”
Another study from this session, presented by Biagio Ricciuti, MD, of Dana-Farber Cancer Institute, focused on clinical outcomes of patients with KRAS-mutated NSCLC. All 416 patients included in the analysis had metastatic NSCLC harboring the KRAS G12C mutation. Using Project GENIE data, Ricciuti and colleagues found that patients treated with first-line anti-PD-L1/PD-1 immunotherapy had a median overall survival of 15 months. For patients treated with first-line chemotherapy, the median overall survival was 13.5 months.
When Ricciuti and colleagues examined outcomes in patients with co-occurring tumor mutations, they found that the co-occurrence of KRAS and STK11 mutations was associated with significantly worse survival outcomes in patients treated with immunotherapy, but not in patients who were treated with chemotherapy. In addition, the co-occurrence of KRAS mutation with KEAP1 mutation was associated with significantly worse outcomes in patients receiving chemotherapy. KRAS and KEAP1 mutation co-occurrence was also associated with shorter survival after immunotherapy, although this difference was not statistically significant.
“Our study suggests that concurrent genomic alterations in STK11 and KEAP1 define unique subsets of KRAS G12C-mutated NSCLC with inferior outcomes to standard of care therapies,” said Ricciuti. He noted that the efficacy of alternative therapies, such as KRAS inhibitors, in these populations remains to be determined.
Additional applications of AACR Project GENIE
Data from AACR Project GENIE was also leveraged to develop an algorithm for estimating the date of disease recurrence in patients with colorectal or lung cancers, according to a presentation by Jessica Lavery, MS, of Memorial Sloan-Kettering Cancer Center (MSKCC).
Beyond aiding discovery science, the database has also been used to validate single-institution findings, as exemplified by a study presented by Sarah Suehnholz, PhD, a senior scientist at MSKCC. Suehnholz used Project GENIE data to validate clinically actionable targets identified in the OncoKB database. Notably, data from both databases revealed a marked increase in the number of clinically actionable gene alterations between 2018 and 2021 due to new drug approvals, additional indications for existing drugs, and a greater understanding of cancer mutations. This expansion highlights the continued growth of the precision medicine field.
What’s next?
As the precision medicine field moves forward, how might AACR Project GENIE evolve? Trevor Pugh, PhD, member of the AACR Project GENIE Genome and Analysis Working Group, and session moderator Bedard spoke to potential future directions of the database.
“[Transcriptome data] is probably the most informative piece of data we could add,” Pugh said, explaining that it would be “enormously informative about a range of therapies.” Additional data types requested by the audience included imaging data, radiomics, NanoString data, and expansion of pediatric data.
Pugh predicted that clinical trial design, validation of individual studies, and continued discovery will be key applications of Project GENIE as it continues to evolve.
Bedard also noted plans to expand Project GENIE by including data from additional institutions. “There are definitely plans to grow GENIE,” he said. “That’s definitely something to stay tuned for.”