Recent Advances in Colorectal Cancer Research
Colorectal cancer is the second leading cause of cancer death in the United States. More than 50,000 people are estimated to have died from colorectal cancer in the United States last year, according to federal statistics.
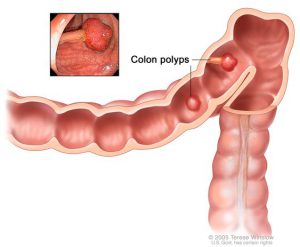
Colorectal cancer typically begins as a slow-growing, noncancerous polyp which, over time, can progress to invasive cancer. If a cancerous polyp isn’t removed, it can penetrate the lining of the large intestine, allowing the cancer to spread to other organs through blood or lymph vessels. With screening, it is possible to detect and remove polyps before they become cancerous. An increase in colorectal cancer awareness and screening has most likely contributed to the overall reduction in colorectal cancer incidence in the last 30 years.
As March is Colorectal Cancer Awareness Month, we’ve put together a selection of recent colorectal cancer studies across the AACR portfolio along with screening recommendations and risk factors associated with this disease.
An improved method to stratify colorectal cancer patients for prognosis
While screening may help to identify patients with colorectal cancer at earlier stages, stratifying these patients into appropriate risk categories, which may guide their treatment and monitoring, is an area of active research.
The current gold standard used for the prognostic stratification of colorectal cancer patients is the Tumor Node Metastasis (TNM) staging system, a clinical method that incorporates tumor size, involvement in regional lymph nodes, and distant metastasis. TNM staging helps classify the tumor into five main stages – stage 0 through stage 4 – to describe the size of the tumor and the extent of its spread.
Another method for patient stratification is Immunoscore. This method utilizes quantification of the density of tumor-infiltrating T cells at the tumor core and its invasive margin to generate an overall score. There was a significant difference in the risk of five-year recurrence between patients with stage 2 colorectal cancer stratified as having high- and low-risk by Immunoscore, according to a previous study.
An independent prognostic feature of colorectal cancer is the presence of tumor buds, or small isolated clusters of cancer cells. Tumor buds have been associated with poor clinical outcomes in a variety of colorectal cancer studies, which are summarized in this review.
The aim of a study recently published in Cancer Immunology Research was to develop a method for risk stratification of colorectal cancer patients by combining multiple factors of prognostic significance. Utilizing data from 114 patients with stage 2 colorectal cancer, the researchers used machine-learning algorithms to develop the Tumor Bud-Immuno Spatial Index (TBISI). The model stratifies patients into high- and low-risk categories of disease-specific death through the combined integration of tumor buds, T-cell infiltration, and their spatial relationship to each other.
The researchers found that TBISI was more than four times and more than twice as effective in the stratification of patients into high- and low-risk groups compared to TNM staging and the study’s version of Immunoscore, respectively. Validation analyses in two independent cohorts confirmed that TBISI was more effective at risk stratification than the two standard methods.
“We found that our combinatorial method was superior to the current prognostic staging systems in defining stage 2 colorectal cancer patient prognosis,” said first author Ines Nearchou, a PhD student at the University of St. Andrews School of Medicine in North Haugh, Scotland, in an AACR press release. “After further validation in larger studies, this index could be translated into routine clinical classification of stage 2 colorectal cancer as well as other solid tumor types, thus providing a more precise prognosis with the ultimate goal of improving patient care.”
Misdiagnosis may be common for patients with young-onset colorectal cancer
Colorectal cancer mostly affects older patients, as nearly 80 percent of new diagnoses are in those aged 55 and older. However, colorectal cancer rates are on the rise in younger adults. According to a recent study, among adults aged 20-29, the rates of colon cancer incidence increased by 2.4 percent per year from the mid-1980s to 2013, and the rates of rectal cancer incidence increased by 3.2 percent per year from 1974 to 2013.
A recent study, which was presented at a media preview of the AACR Annual Meeting 2019, analyzed responses from a comprehensive survey of over 1,000 young-onset colorectal cancer patients and survivors. Of these participants, 57 percent were diagnosed between ages 40 and 49; 33 percent were diagnosed between ages 30 and 39; and about 10 percent were diagnosed before age 30.
The study, which was led by Ronit Yarden, PhD, MHSA, director of medical affairs at the Colorectal Cancer Alliance, found that over 70 percent of respondents were diagnosed with late-stage disease. As such, these patients were subjected to aggressive therapies and experienced a substantial decrease in their quality of life. In contrast, patients over 50 are significantly more likely to be diagnosed at earlier stages, which carries a better prognosis.
The majority of these young-onset patients waited between three and 12 months after symptom onset before seeking medical help, partially because they did not recognize their symptoms as being related to colorectal cancer. Furthermore, 67 percent of patients saw at least two physicians – with some patients seeing as many as four physicians – before receiving a diagnosis of colorectal cancer.
According to the study, the most common misdiagnoses for colorectal cancer were inflammatory bowel disease or hemorrhoids, which can share similar symptoms.
“We need to increase awareness that colon cancer affects not only elderly people but also younger ones,” said Yarden in a nbcnews.com story. “Of all the different types of cancer, colon cancer is one of the most preventable ones and also, if misdiagnosed and then discovered at a later stage, one of the most deadly ones. We need that information to trickle down to both patients and physicians.”
Prevention of colorectal cancer through screening and lifestyle
While the five-year relative survival is around 65 percent for all patients with colorectal cancer, for those with localized disease, it is nearly 90 percent. Regular screenings for the disease, which can include removing benign polyps before they become cancerous, can help to identify colorectal cancer at an earlier stage or prevent the disease altogether.
The U.S. Preventive Services Task Force recommends that adults age 50 to 75 be screened for colorectal cancer, and some professional societies recommend starting regular screening at age 45. Recommended screening methods are fecal occult blood testing, sigmoidoscopy, or colonoscopy, with varying times between tests, depending on the type of screening.
Despite these recommendations, 38 percent of adults ages 50-75 were not up to date with colorectal cancer screening, according to data from 2015. Screening rates varied by race – only 48 percent of American Indian/Alaskan Natives were up to date with their screening, while 64 percent of whites were up to date. Additionally, colorectal cancer screening rates have been shown to vary widely throughout the United States, a finding which was highlighted in a recent study published in Cancer Epidemiology, Biomarkers & Prevention.
Recommendations from the National Comprehensive Cancer Network (NCCN) and the United States Multi-Society Task Force (MSTF) on colorectal cancer indicate that individuals at increased risk, such as those with a family history of colorectal cancer or those that carry a genetic mutation that causes Lynch syndrome, should begin screening earlier than age 45. Read this sidebar in the 2018 AACR Cancer Progress Report to learn more.
Finally, several lifestyle factors have been associated with an increased risk of colorectal cancer, such as diets rich in red/processed meat, the consumption of alcohol, and obesity. Modification of these lifestyle factors can help to reduce our risk of colorectal cancer.
For more information on recent colon cancer research, check out this collection of journal articles selected by the AACR editors about studies in the field spanning across the AACR journals.





data about colorectal cancer in this website are so useful and important