Study Predicts Uterine Cancer Incidence May Significantly Increase by 2050
Incidence-based mortality is also projected to increase with disproportionately higher rates for Black women compared with white women.
Incidence and mortality rates for most cancer types have been on the decline in the United States in recent years, thanks to advances in prevention, early detection, and treatment. However, a new study found that these rates for uterine cancer are projected to increase significantly over the next three decades in the United States. Further, incidence-based mortality, or the death rate among patients diagnosed in a given time frame relative to the death rate of the general population, is expected to be nearly three times higher in Black women compared to white women by 2050.

The study was published in Cancer Epidemiology, Biomarkers & Prevention, a journal of the American Association for Cancer Research (AACR).
“Overall, uterine cancer is one of the few cancers where both incidence and mortality have been increasing, and prior studies have consistently shown significant racial disparities among Black and white women,” said the study’s lead author, Jason D. Wright, MD, chief of the Division of Gynecologic Oncology at Columbia University. “Understanding future trends will help inform the development of robust strategies to reduce the burden and improve outcomes.”
Examining Current Trends in Uterine Cancer
Cases of uterine cancer have increased an average of 0.7% each year between 2013 and 2022, and age-adjusted death rates increased 1.6% annually between 2014 and 2023, according to the Surveillance, Epidemiology, and End Results (SEER) Program at the National Cancer Institute (NCI). Black women are disproportionally affected with a death rate from uterine cancer that is about twice as high compared to women of other races or ethnicities.
As part of the NCI’s Cancer Intervention and Surveillance Modeling Network (CISNET), which is working to model trends for several different cancer types, Dr. Wright and his colleagues built the Columbia University Uterine Cancer Model (UTMO). This natural history model of uterine cancer simulates the trajectories for incidence and mortality based on characteristics from a sample population, taking into account factors such as age, race, birth cohorts grouped in 10-year intervals, stage, and histologic subtype—for example, endometrioid uterine cancer is a more common subtype vs. non-endometrioid cancers, which tend to have a worse prognosis. Survival estimates are based on current available treatments and did not account for potential advances in therapeutics.
After inputting the criteria into UTMO, Dr. Wright and his team tested its accuracy by predicting the median age of diagnosis, survival rate, and distribution of diagnosis by stage for uterine cancer in 2018. They found that the projections from UTMO were comparable to the actual SEER data from that year, validating the model.
Back to the Future of Uterine Cancer
Following this, they estimated the future rates of uterine cancer based on publicly available sources through 2018. Incidence was projected to increase from 57.7 cases per 100,000 in 2018 to 74.2 cases per 100,000 in 2050 for white women, and from 56.8 cases per 100,000 to 86.9 cases per 100,000 for Black women. Incidence-based mortality was projected to increase from 6.1 per 100,000 to 11.2 per 100,000 among white women, and from 14.1 per 100,000 to 27.9 per 100,000 among Black women.
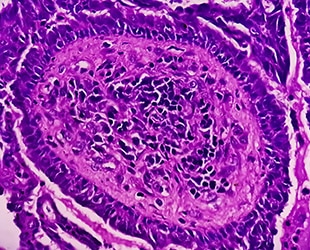
Further, while the incidence of endometrioid tumors is projected to increase considerably in both Black (34.2 per 100,000 to 50.5 per 100,000) and white (49.2 per 100,000 to 63.4 per 100,000) women, the increased incidence of non-endometrioid tumors was more significant in Black (from 22.5 per 100,000 to 36.3 per 100,000) than white (from 8.5 per 100,000 to 10.8 per 100,000) women.
“There are likely a number of factors that are associated with the increased burden of uterine cancer in Black women,” Dr. Wright said. “They more commonly have aggressive types of uterine cancer, face delayed diagnosis resulting in later-stage disease at diagnosis, and there are often delays in their treatment.”
Since obesity is a known risk factor for uterine cancer and hysterectomy is known to reduce the risk of uterine cancer, the researchers also used the model to see whether uterine cancer rates would be affected should obesity continue to increase and hysterectomies decrease. In that instance, incidence and mortality rates for uterine cancer would rise even more drastically for both white and Black women. Dr. Wright acknowledged that increased use of obesity treatments like GLP-1s could instead cause obesity rates to decline, but he said it is hard to predict if that will be the case over the next 30 years. Meanwhile, he explained that hysterectomy rates have been declining due to the availability of nonsurgical treatments for gynecologic disease with projections expecting their rate to further decline 25.7% from 2020 to 2035.
Dr. Wright and his colleagues also performed a stress test of the model by incorporating hypothetical screening and intervention methods that could detect uterine cancer and precancerous changes prior to clinical diagnosis. The screening and intervention methods were most effective when introduced at age 55 with declines in cancer incidence that lasted up to 15 years in white women and up to 16 years in Black women.
“The stress testing suggests that if there was an effective screening test, we may be able to substantially reduce the burden of disease,” Dr. Wright said. “While there is presently no screening or prevention that is routinely used for uterine cancer, we are currently examining the potential impact of integrating screening for this cancer into practice.”
The bottom line, according to Dr. Wright: “There is an urgent need to develop strategies to reduce the incidence of uterine cancer and to promote early detection.”