Pediatric Cancer’s Aftershocks: The Challenges for Survivors Beyond Childhood
When a child overcomes cancer, it is a moment for heartfelt celebration, and those hard-won moments are worth fighting for. But while every case of pediatric cancer remission marks a victory for cancer research, the fight for patients with pediatric cancer doesn’t stop there. As they age, children who survive cancer face heightened risks of health issues relative to the rest of the population, and recent research shows that continued vigilance is necessary throughout survivors’ lives to keep adverse conditions at bay. Longer lives are a good thing, and now, researchers are committed to improving the quality of life.
First Steps: Facing an Initial Diagnosis of Pediatric Cancer
Childhood cancer is anomalous almost by definition; as a disease of accrued mutations and biological entropy, cancer mostly affects older adults, with incidence increasing directionally with age. But though comparatively rare, childhood cancer does happen, mostly as the result of acquired mutations. An estimated 9,620 children were diagnosed with cancer in the United States last year, of whom about 1,040 likely succumbed to their disease.

Thankfully, the outlook for patients is brightening: the five-year survival rate for childhood cancers has recently climbed to 83-88%, a significant improvement from the 1970s’ 58-68%. With new research, treatment options have expanded, but generally, childhood cancer is treated with chemotherapy drugs; radiation therapy; surgical tumor removal; and targeted therapies and immunotherapies, especially CAR-T cell therapy.
Because newer cancer treatments have improved survival for childhood cancer patients, more survivors face the challenges of long-term effects from the disease and treatments, including risk of cancer recurrence and certain general risks, such as hearing loss and overall health issues. Thankfully, today’s researchers, by using data from a growing pool of survivors, are making headway on ameliorative strategies for all these challenges.
Heavy Metal Is Bad for Hearing
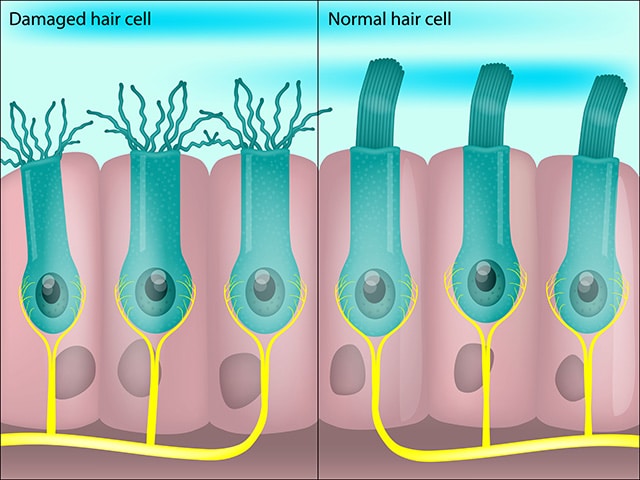
Some of the most common chemotherapy drugs function thanks to the active ingredient platinum: a heavy metal that, when administered as chemotherapy drugs like cisplatin, causes fatal cell damage at a disproportionately high rate in rapidly dividing cells. But not only is platinum-based chemotherapy notoriously toxic—it’s also highly ototoxic, meaning that the drugs damage hearing up to and including hearing loss, for which pediatric cancer patients are at especially high risk. Platinum-based drugs can cause the fine hairs within the inner ear—structures that are essential for hearing—to degenerate, and because those hairs do not naturally regrow, the effects can be permanent.
For pediatric cancer patients vulnerable to hearing loss from platinum-based drugs, there is a critical need to understand and combat a potentially lifelong disability. But a recent study in the American Association for Cancer Research (AACR) journal Cancer Research Communications offers a hopeful path forward: The research team found that one key enzyme, APE2, caused fatal mitochondrial damage in the inner-ear hair cells when treated with cisplatin due to an interaction with the MYH9 protein. Led by the Cleveland Clinic’s Lerner Research Institute’s Jianhong Lin, MD, PhD, and Jianjun Zhao, MD, PhD, the study found that, by removing APE2, the team could successfully protect the cochlear cells against cisplatin damage.
In 2022, the FDA approved the sodium thiosulfate drug (Pedmark) as an anti-ototoxicity therapy for children receiving chemo, but because sodium thiosulfate protects hearing by countering cisplatin directly, it can reduce chemotherapy’s anticancer effects—which restricts sodium thiosulfate’s approved use to local, nonmetastatic cancers. Lin, Zhao, and their co-authors hope that their proposed therapy, which leaves cisplatin’s anticancer mechanisms intact, could provide hearing protection for many more patients.
Life Beneath the Sword of Damocles
Survivors of childhood cancer live with the knowledge that they are at a greater risk of cancer coming back. A recent study found that, of 229 adult survivors of pediatric cancer, a full third experienced a high fear of recurrence or developing new cancer—and of that third, about half experienced very high levels of fear, which were associated with mood disorders like anxiety and depression, as well as other negative outcomes, like unemployment and elevated health concern.
One study places the risk of pediatric cancer survivors developing a subsequent malignancy at any point after their primary diagnosis at 4.2%, and some of these subsequent malignancies can be quite deadly. That same study found that, of the 4.2% of the pediatric cancer survivor cohort who developed subsequent malignant neoplasms, 38% died from those malignancies. The threat of these secondary cancers also persisted for a long time, with most of them occurring within the second decade following initial treatment at the earliest.
But as the saying goes, an ounce of prevention is worth a pound of cure. Because cancer recurrence is a well-known risk, survivors of childhood cancer can be monitored with frequent screenings. One study found that adherence to a regular, proactive screening schedule for colorectal cancers reduced the risk of mortality in childhood cancer survivors by 73% from colon cancer, an indication that surveillance and monitoring may help catch recurring cancers at earlier, more treatable stages.
Biological Clocks Ticking Faster
If cancer itself is a disease of aging in certain ways, then it makes intuitive sense that childhood cancer and the treatment thereof are known drivers of premature aging. Cancer therapies stress the body’s systems, and with biological stress comes the risk of chronic conditions. Even in young patients, whose youth might otherwise protect them against developing age- and stress-associated conditions, the burdens of treatment lead to increased risks of several chronic health issues for which survivors and their health care providers must remain on the lookout.
Cholesterol issues, also known as dyslipidemia, affect the health of many Americans. By the measure of total cholesterol levels exceeding 240 mg/dL, 17% of adults over 20 have dyslipidemia, but the risk is higher for survivors of childhood cancer. According to one study, survivors were 56% more likely to develop dyslipidemia than their cancer-free siblings.
Chronic kidney disease, a frequent comorbidity of dyslipidemia, also occurs at a significantly higher rate among survivors of childhood cancer than in the general population. One analysis of childhood cancer survivors found that their risk of developing chronic kidney disease was roughly double that of the control cohort; the same study found that hypertension, a major driver of mortality, also affected survivors of childhood cancer at double the rate of the general population.
Survivors of childhood cancer may also face poorer overall health in general. A study aiming to assess the accelerated aging of childhood cancer survivors found that, of eight conditions that tend to develop later in life—namely, breast cancer, colorectal cancer, glial tumors, sarcomas, heart failure, coronary heart disease/myocardial infarction, stroke, and valvular disease—20% of the general population developed at least one of the conditions by age 65. However, childhood cancer survivors hit the same benchmark threshold a full 17.7 years earlier. Put another way, the general health of a 47-year-old American adult who had cancer as a child is roughly equivalent to that of a 65-year-old American adult who didn’t have childhood cancer—a marked acceleration in biological aging.
The Psychosocial Costs of Cancer
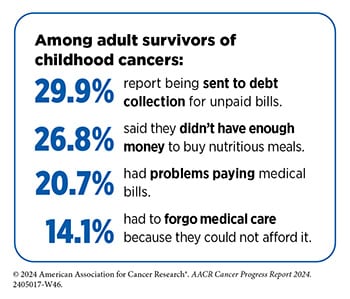
The costs of cancer don’t just include tolls on one’s health; diagnosis often means a significant financial burden as well. Young families may not have the same health care savings as older individuals, potentially making them more vulnerable to the financial toxicity that can accompany a cancer diagnosis. That toxicity has the potential to continue to bear on survivors, who, as they grow up, must continue to pay for screenings and the other health care costs associated with the comorbidities that come with having survived cancer. Further, the potential restrictions placed on educational and/or career attainment as a result of cancer treatment may limit the earning potential that might otherwise offset such financial difficulties.
Between the fear attendant on receiving a diagnosis and the disruptions of undergoing treatment—missed school, limited socializing, distorted self-image from treatment’s side effects—children with cancer are much more likely to develop psychiatric disorders like anxiety, depression, bipolar disorder, and PTSD, among others. These survivors also tend to struggle with addictions (themselves comorbidities of many mental illnesses), placing them at risk of alcohol and tobacco’s deleterious health effects. In addition to the care and guidance of mental health professionals to navigate these vicissitudes, childhood cancer survivors also require a continuation of support and empathy. The compassion and care of robust support networks can go a long way in reducing the burden of mental health struggles.
Looking Forward to Better Outcomes
Cancer research continues to make the necessary strides toward improving not just the treatment of pediatric cancer but also the long-term care of its survivors. By shedding much-needed light on childhood cancer survivors’ increased risk of all manner of health conditions, researchers continue to give both survivors and their health care providers the tools they need to develop informed strategies for health maintenance in the long term.
And with every new understanding of the precise causes of long-term health issues comes an opportunity for a new strategy to improve survivors’ health—especially as the percentage of those who survive a childhood cancer diagnosis continues to grow on the heels of better cancer treatments.
Learn more about childhood cancers and how the AACR is supporting research in this area on the AACR’s Childhood Cancer Awareness Month page.