Tracking the History of Tucatinib for Breast Cancer Treatment at SABCS
Every cancer plays by signals, and in human epidermal growth factor receptor 2 (HER2)‑positive breast cancer, those signals are amplified through the HER2 receptor that functions like an “always‑on” antenna. The result is a fast‑moving disease subtype that historically spreads early and often to the brain, where the blood-brain barrier limits drug access and undermines systemic control.
The HER2 protein is overexpressed in roughly 17% of breast cancers and is associated with a poorer prognosis. Among patients with metastatic HER2‑positive disease, five‑year survival rates have been estimated at about 41-47% depending on hormone receptor (HR) status, which underscores why clinicians keep pushing for better, earlier, and more brain‑relevant therapies.
Early clinical data published in American Association for Cancer Research (AACR) journals and data from the HER2CLIMB trials presented at the San Antonio Breast Cancer Symposium (SABCS) over the years have cemented the role of tucatinib (Tukysa) in treating HER2-positive breast cancer. A drug that started off in the realm of salvage therapy and—after much study—was approved to extend frontline control of HER2-positive breast cancer.
Tucatinib is an oral, HER2 kinase inhibitor designed to curtail HER2 signaling—trying to give that “always-on” signaling antenna some down time. Preclinical studies have shown that tucatinib is a selective inhibitor of HER2, largely sparing the epidermal growth factor (EGFR), another cell-surface protein that drives growth signals in normal tissues. Inhibiting EGFR broadly can disrupt the pathways for cell division in the skin and gastrointestinal lining, which is why older tyrosine kinase inhibitors (TKIs) often cause severe rashes and diarrhea.
Early Clinical Trials Testing Tucatinib
The first clinical trial of tucatinib—then known as ONT‑380—followed a standard dose escalation approach in patients with metastatic HER2‑positive breast cancer, most of whom had received several prior treatments. According to the results of this 2013 study, which was published in Clinical Cancer Research, the researchers found that tucatinib had a more favorable toxicity profile compared with either dual EGFR/HER2 or pan-HER TKIs that existed at the time. There were signals that tumors could shrink with tucatinib alone, and side effects were often manageable, based off the information in the study. The more serious side effects at higher doses were elevations in liver enzymes; those usually improved when the dose was held or reduced, and patients could continue treatment afterward.
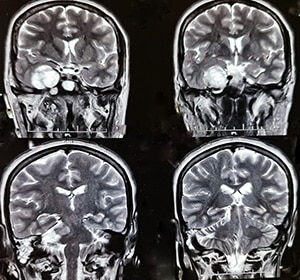
Another clinical trial, which put brain metastasis to the forefront, enrolled only HER-positive breast cancer patients with progressive, measurable brain metastases. The treatment was a combination of tucatinib with trastuzumab (Herceptin), a HER2-targeted antibody, leaving out chemotherapy to isolate the effect of the targeted drug. The study explored two dosing schedules—300 mg twice daily and 750 mg once daily—and determined both were feasible, with the maximum tolerated dose set at 300 mg twice daily for the twice-daily arm.
The results showed that the twice-daily schedule maintained drug levels above the threshold needed for HER2 inhibition, whereas once-daily dosing produced higher peaks but lower troughs. The clinical benefit rate (CBR), which was the percentage of patients that showed complete response, partial response, or stable disease for 16 weeks in the case of this trial, was measured for both arms. The twice-daily cohort showed a CBR of 35% and the once-daily cohort showed a CBR of 53%, and intracranial responses were documented in three patients. Some participants remained on therapy for over a year despite prior treatment that included lapatinib (Tykerb) and neratinib (Nerlynx). These results compared favorably to historical central nervous system (CNS) response rates with other HER2-targeted TKIs like lapatinib. While the sample size was small and the trial was not designed for definitive efficacy comparisons, it was a step closer to understanding what tucatinib could achieve in terms of meaningful disease control in the brain without chemotherapy.
HER2CLIMB at SABCS 2019: Survival Gains, Including in Brain Metastases
The next step in tucatinib’s journey was a pivotal phase II trial—HER2CLIMB—which was designed to seek regulatory approval. This global, randomized study compared adding tucatinib to the standard combination of trastuzumab and capecitabine (Xeloda) versus adding a placebo to that same standard regimen for patients previously treated with trastuzumab, pertuzumab (Perjeta), and ado-trastuzumab emtansine (T-DM1, Kadcyla).
The results of this trial, presented at SABCS 2019, showed that tucatinib prolonged progression‑free survival (PFS) by 46% compared to the control arm. In the brain‑metastasis subset—which was 47% of the patients—those treated with tucatinib had a 52% reduction in disease progression or death compared to the control arm. Overall, the study showed that tucatinib reduced the risk of death by 34% compared with trastuzumab plus capecitabine. These results led to the FDA’s approval of tucatinib in 2020, which explicitly included “patients with brain metastases” in the indication.
Alongside the FDA approval, tucatinib was also approved by the Australian, Canadian, Singaporean, and Swiss regulatory agencies as well. This was because tucatinib was the first new molecular entity reviewed under Project Orbis—an international, parallel review pathway—that was used to help accelerate global drug development. This marked the first time the FDA collaborated with Singaporean and Swiss regulatory agencies.
HER2CLIMB-05 at SABCS 2025: Frontline Use and Longer PFS
As tucatinib moved from salvage to established later‑line option, a logical question emerged: could the same biology be leveraged earlier to prevent or at least postpone disease progression and extend frontline control? That was the hypothesis that drove HER2CLIMB‑05, a phase III study testing tucatinib added to standard first‑line maintenance therapy—trastuzumab plus pertuzumab—after induction chemotherapy, explained Erika Hamilton, MD, director of Breast Cancer Research at Sarah Cannon Research Institute (SCRI), who presented the HERCLIMB-05 study data at SABCS 2025.
“Through the HERCLIMB-05 trial, we found that the addition of tucatinib to the standard of care represents an enhanced first-line maintenance therapy option for patients with HER2-positive metastatic breast cancer, providing an opportunity to prolong time to disease progression and time off chemotherapy,” said Hamilton in a press release.
The study enrolled 654 patients who were randomly assigned 1:1 to tucatinib versus placebo with trastuzumab and pertuzumab, framing the maintenance concept as a potential chemotherapy‑free way to strengthen frontline control. The patients who received tucatinib had a PFS of over two years—an improvement of 8.6 months compared with the patients in the control arm.

Hamilton explained that these results, alongside recent data from the PATINA trial—where incorporating palbociclib (Ibrance) into the treatment regimen for HR-positive, HER2-positive metastatic breast cancer showed a 15-month improvement in PFS—support a shift toward more personalized first-line maintenance strategies for patients with this breast cancer subtype.
To appreciate why HER2CLIMB‑05 matters, it helps to recall that frontline HER2‑positive metastatic care has plateaued over the recent decade. Since 2012, the standard of care for this subtype has remained unchanged, with most patients relapsing within two years, said Hamilton. Bringing tucatinib into that maintenance window was an attempt to extend the runway before progression and improve quality of life by keeping chemotherapy off the maintenance stage, she explained. The HER2CLIMB‑05 study suggests that this strategy works at least on PFS—the first proof that tucatinib’s chemistry can add value before the disease evolves through multiple lines.
Tucatinib’s arc—early human tolerability, dedicated CNS trials, pivotal later‑line efficacy with explicit intracranial benefit, and now frontline maintenance—reflects the consistent buildup of data to answer the same clinical question posed at different stages of disease: can a HER2‑selective therapeutic safely deepen the HER2 blockade in the brain?
The preliminary results for intracranial efficacy documented in HER2CLIMB showed that tucatinib may work inside the CNS, and the frontline maintenance benefit of HER2CLIMB‑05 suggests that earlier exposure may prolong time before any progression, potentially shortening the window during which new brain lesions typically emerge. Among the 12.2% of patients with brain metastases at baseline, tucatinib nearly doubled the median central nervous system-PFS, which is the time taken for the cancer to progress to the brain or death from any cause—from 4.3 months to 8.5 months; this was however not statistically significant.
The story isn’t done yet—researchers know that this is just the beginning—“Central nervous system-PFS was a secondary endpoint and findings regarding the delaying of brain metastasis are preliminary,” cautioned Hamilton, adding that 54% of the patients in the tucatinib arm remained on study treatment at the data cutoff of this analysis.
Science rarely moves in leaps; it advances in linked, tested steps—and tucatinib is a case study. The HER2‑selectivity quest through preclinical proof, investigating a safe dose, studying intracranial activity in a brain‑metastasis trial, and a pivotal randomized study that drove rapid global approvals, to HER2CLIMB‑05 pointing toward frontline maintenance, were all necessary steps that built on each other, reflecting a coordinated, worldwide effort against HER2‑positive metastatic breast cancer.
For those who have registered for the symposium, sessions may be viewed on the SABCS virtual platform through March 31, 2026.