CAR T-cell Therapy Approved for Rare Lymphoma
Lisocabtagene maraleucel was granted approval for adults with treatment-resistant marginal zone lymphoma.
The U.S. Food and Drug Administration (FDA) has approved lisocabtagene maraleucel (Breyanzi) for adults with relapsed or refractory marginal zone lymphoma (MZL) who have received at least two prior lines of systemic therapy.
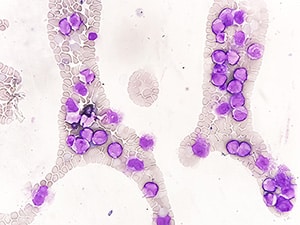
Lisocabtagene maraleucel is an autologous chimeric antigen receptor (CAR) T-cell therapy, a type of immunotherapy in which clinicians remove the patients’ T cells via leukapheresis, send them to be genetically engineered, and infuse the modified T cells back into the patient. Once modified, the T cells express a CAR to enhance their targeting of CD19, which is expressed on the surface of both cancerous and normal B cells. The binding of CAR T cells to B cells induces CAR T-cell activation and proliferation, leading to inflammation and the death of CD19-expressing B cells.
This approval is the newest lymphoma indication for lisocabtagene maraleucel, which was originally approved for B-cell lymphomas in 2021 and has since been approved for several other lymphoma types. Lisocabtagene maraleucel is the first CAR T-cell therapy to be approved for MZL.
The approval for this indication is based on results from the FL-MZL cohort of the TRANSCEND clinical trial. In the open-label, single-arm, multicenter phase II clinical trial, 77 patients with MZL—who had stopped responding to at least two previous lines of systemic therapy or had experienced disease relapse after a hematopoietic stem cell transplant—underwent leukapheresis, and 67 patients of those 77 received lisocabtagene maraleucel.
Among the 77 patients who underwent leukapheresis, 84.4% experienced treatment responses, and 55.8% experienced complete responses. The median duration of response was not reached, meaning that, by the time of follow-up, more than half of the patients continued to have responses to treatment.
The prescribing information for lisocabtagene maraleucel includes a boxed warning for the treatment’s risk of causing three severe and potentially life-threatening side effects: cytokine release syndrome, neurologic toxicities, and subsequent T-cell malignancies. The warning cautions clinicians to monitor patients for signs of these side effects, and it also instructs them not to administer lisocabtagene maraleucel to patients with active infection or inflammatory disorders.
The recommended lisocabtagene maraleucel dose is 90-110 × 106 CAR-positive viable autologous T cells with equal distribution of CD4-positive and CD8-positive T cells. After they have received lymphodepleting chemotherapy to clear their existing immune systems, patients receive lisocabtagene maraleucel as an intravenous infusion.
Lymphoma is a cancer that forms in the cells of the lymphatic system throughout the body. According to federal statistics, it was estimated that 80,350 individuals would be diagnosed with non-Hodgkin lymphoma (the predominant variety of lymphoma) and 19,390 patients would die of the disease in the United States in 2025. Marginal zone lymphoma—which occurs in the regions where the lymphatic system interacts with other body systems— accounts for an estimated 5% to 10% of lymphoma cases. As an “indolent” cancer, MZL often grows slowly, but early relapse in patients with MZL is associated with a risk of death almost 20 times that of patients without early disease progression.
The FDA rendered its decision on December 4, 2025. Check this resource for updated information on all therapeutics regulated by the FDA.