A New First-line Option for Metastatic Breast Cancer
Fam-trastuzumab deruxtecan-nxki (T-DXd) with pertuzumab was approved to treat metastatic HER2-positive breast cancer.
The U.S. Food and Drug Administration (FDA) has approved fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu) in combination with pertuzumab (Perjeta) for patients with newly diagnosed human epidermal growth factor receptor 2 (HER2)-positive breast cancer that has either metastasized or cannot be removed with surgery.
Concurrently, two tests were approved for evaluating a tumor’s HER2 status: the PATHWAY test and the VENTANA test.
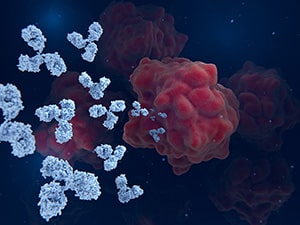
T-DXd is an antibody-drug conjugate (ADC) that targets HER2, which is expressed in HER2-positive breast cancer cells at greater levels than in healthy cells. Once the antibody binds to a cell expressing HER2, the ADC enters the cell, and the toxic drug component kills the cell. Pertuzumab is a monoclonal antibody that binds to HER2 and inhibits its activity.
The approval of T-DXd for untreated metastatic or unresectable HER2-positive breast cancer provides newly diagnosed patients with a new first-line treatment option that may be more effective than the current standard of care, which combines taxanes (a kind of chemotherapy) with HER2-targeted monoclonal antibodies. Experts discussed how this new first-line option fits into the therapeutic landscape for metastatic breast cancer at the San Antonio Breast Cancer Symposium 2025; read more about their discussion on the AACR blog.
The new approved indication for T-DXd is based on results from the randomized, three-arm, multicenter phase III DESTINY-Breast09 clinical trial. The trial enrolled 1,157 adults with metastatic or advanced HER2-positive breast cancer. Patients were excluded if they received prior chemotherapy or HER2-targeted therapy, although an exception was made if patients received chemotherapy or HER2-targeted therapy more than six months before their cancer metastasized.
Patients were randomly assigned 1:1:1 to receive one of three treatments: T-DXd plus pertuzumab; a combination of a taxane, trastuzumab (Herceptin), and pertuzumab (THP); or an investigational therapy. The efficacy of T-DXd was measured against that of THP.
Patients in the T-DXd arm were 44% less likely to experience disease progression than patients in the THP arm during the follow-up period of about 45 months. The median progression-free survival (PFS) was 40.7 months in the T-DXd arm, whereas patients in the THP arm had a median PFS of 26.9 months. The percentage of patients whose tumors responded to treatment was also higher in the T-DXd arm (87%) than in the THP arm (81%).
The prescribing information for T-DXd includes a boxed warning because the drug can cause potentially fatal interstitial lung disease (ILD) and pneumonitis, as well as embryo-fetal harm.
The recommended dose of T-DXd is 5.4 mg/kg, with 840 mg of pertuzumab, as an initial dose. Every three weeks thereafter, each subsequent dose of T-DXd dose is 5.4 mg/kg with 420 mg of pertuzumab. Treatment should be continued until either disease progression or unacceptable toxicity occurs.
Breast cancer is the most common non-skin cancer in women, and federal statistics estimate that, in 2025, 316,950 individuals were diagnosed with it and 42,170 died of the disease. HER2-positive breast cancer accounts for about 13% of all U.S. cases.
The FDA rendered its decision on December 15, 2025. Check this resource for updated information on all therapeutics regulated by the FDA.