Combination Therapy With Antibody-drug Conjugate Approved for Multiple Myeloma
The FDA approved the BCMA-targeted antibody-drug conjugate belantamab mafodotin-blmf as part of a combination therapy for adults with refractory or recurrent multiple myeloma.
The U.S. Food and Drug Administration (FDA) has approved belantamab mafodotin-blmf (Blenrep) as a combination therapy with bortezomib (Velcade) and dexamethasone for adults with refractory or recurrent multiple myeloma who have received at least two prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent.
As an antibody-drug conjugate (ADC), belantamab mafodotin-blmf targets the B-cell maturation antigen (BCMA) protein, which is preferentially expressed on mature B cells, including multiple myeloma cells. Once the antibody component of belantamab mafodotin-blmf binds to the protein, the ADC is internalized by the cell, and the toxic small-molecule payload kills the cell.
In August 2020, the FDA granted accelerated approval to belantamab mafodotin-blmf as a monotherapy for adults with multiple myeloma that was refractory to treatment or had relapsed after at least four prior therapies. At the time, the drug was the first on the U.S. market to target BCMA. However, when the phase III DREAMM-3 confirmatory trial failed to demonstrate belantamab mafodotin-blmf’s superiority to existing treatments for this patient population, the approval was withdrawn in March 2023.
The new approval is based on the results from the DREAMM-7 clinical trial. In this open-label, randomized, multicenter phase III trial—which included adults with relapsed or refractory myeloma who had received prior therapy—patients were randomly assigned (1:1) to receive one of two combination therapies: either belantamab mafodotin-blmf, bortezomib, and dexamethasone; or daratumumab (Darzalex), bortezomib, and dexamethasone.
Treatment efficacy was evaluated in 217 patients who had received at least two prior lines of therapy. After a median follow-up of 27.9 months, patients who received the therapy with belantamab mafodotin-blmf were 69% less likely to have experienced disease progression than patients who received the daratumumab-containing regimen (median progression-free survival [PFS] of 31.3 months versus median PFS of 10.4 months, respectively).
Patients who received belantamab mafodotin-blmf were 51% less likely to have died after a median follow-up of 38.7 months compared with those who received daratumumab instead. Median overall survival (OS) was not reached in the belantamab mafodotin-blmf arm—meaning that more than half of those patients were still alive at the time of follow-up—compared with a median OS of 35.7 months in the daratumumab arm.
Due to the risks of ocular toxicity, belantamab mafodotin-blmf was approved with a boxed warning about the potentially harmful changes that the drug can cause in the cornea. Because of these risks, belantamab mafodotin-blmf is only available through a risk evaluation and mitigation strategy.
The recommended dose for belantamab mafodotin-blmf is 2.5 mg/kg once every three weeks—in combination with bortezomib and dexamethasone—for the first eight cycles, followed by 2.5 mg/kg of belantamab mafodotin-blmf as a single agent once every three weeks until disease progression or unacceptable toxicity.
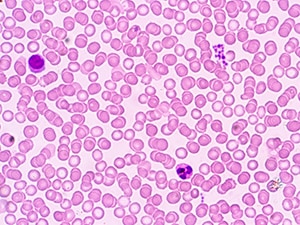
As a comparatively rare form of blood cancer, multiple myeloma forms within the bone marrow when excessive abnormal B cells accumulate and form tumors throughout multiple bones. The National Cancer Institute estimated that, in the United States, 36,110 individuals would be diagnosed with multiple myeloma and 12,030 patients would die of the disease in 2025.
The FDA rendered its decision on October 23, 2025. Check this resource for updated information on all therapeutics regulated by the FDA.