Confronting Stage 3 Lung Cancer With Immunotherapy
The U.S. Food and Drug Administration (FDA) recently approved expanding the use of the immunotherapeutic durvalumab (Imfinzi) to include the treatment of certain patients with the most common form of lung cancer – non-small cell lung cancer (NSCLC).
Specifically, durvalumab is intended for patients with stage 3 lung cancer that cannot be removed surgically and has not progressed after the completion of concurrent treatment with platinum-based chemotherapy and radiotherapy.
Lung cancer is the second-most commonly diagnosed cancer and the leading cause of cancer death in the United States, according to statistics from the National Cancer Institute. More than 220,000 people are diagnosed with the disease each year, and about one-third have stage 3 disease at the time of their diagnosis. NSCLC is classed as stage 3 when the cancer has spread to nearby lymph nodes or other parts of the body near the lungs but has not spread to distant parts of the body.
For many patients with stage 3 lung cancer, surgery is not a treatment option and the cancer is said to be unresectable. Concurrent treatment with platinum-based chemotherapy and radiotherapy, so-called chemoradiotherapy, is often used in this setting. However, five-year survival rates among these patients are only 15 percent, and new treatment options are urgently needed.
The approval of durvalumab for treating unresectable stage 3 NSCLC that has not progressed following the completion of chemoradiotherapy was based on results from the randomized, placebo-controlled, phase III PACIFIC clinical trial, which were published last fall in The New England Journal of Medicine. In brief, the data showed that durvalumab almost tripled the median length of time before disease progressed. Among patients who received durvalumab after chemoradiation, the median time to disease progression was 16.8 months, compared with 5.6 months among those who received placebo.
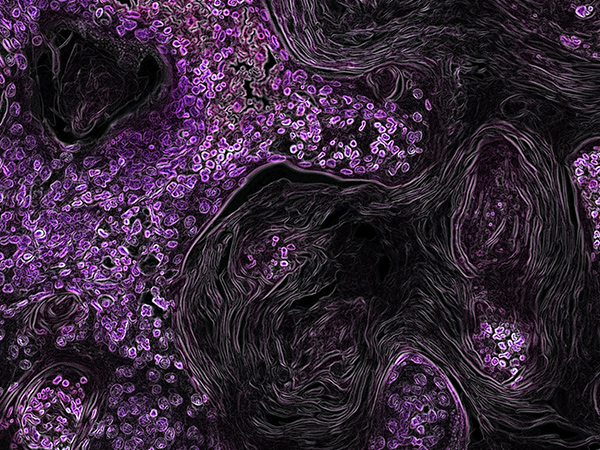
Durvalumab works by releasing a brake on natural cancer-fighting immune cells called T cells. The brake, which is called PD-1, can be triggered by a protein known as PD-L1. Durvalumab prevents PD-L1 from engaging the PD-1 brake, freeing the T cells to destroy cancer cells.
Durvalumab is one of five immunotherapeutics that target the PD-1/PD-L1 braking system to have been approved by the FDA for treating a range of cancer types. The approvals for each of these immunotherapeutics vary, with some overlapping and some unique to a particular agent. For example, durvalumab is the only one of the five to be approved for treating stage 3 cancer. However, all five have been approved for treating bladder cancer, and it is likely that we will see the uses of all these revolutionary anticancer treatments expanded in the near future.
This article was adapted with permission from a post on the AACR’s official blog, CANCER RESEARCH Catalyst.
