Expert Panel Eyes Starting Colorectal Cancer Screening Sooner
Draft recommendation calls for screening at age 45, rather than 50.
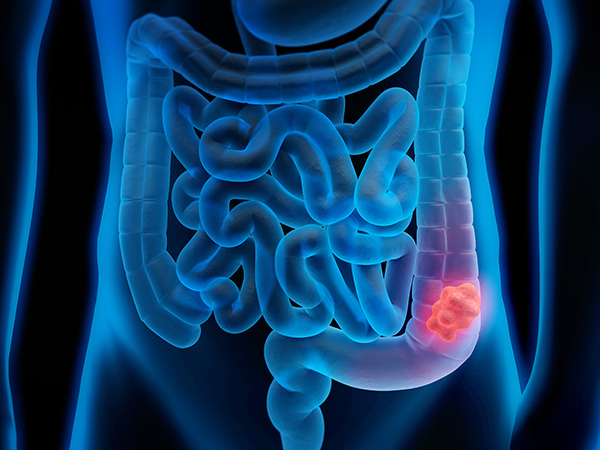
An influential panel of experts has issued a draft recommendation to the federal government that both men and women should start getting screened for colorectal cancer at age 45, five years earlier than the current standard recommendation of age 50.
The U.S. Preventive Services Task Force said it found “adequate evidence” that screening in adults 45-49 would provide “moderate benefit” in terms of reducing deaths from colorectal cancer and increasing life-years gained.
The draft recommendation is open for public comment until November 23, 2020. If the recommendation is finalized by the task force, it would mean that, under the Affordable Care Act, health insurance plans would have to cover colorectal cancer screening from age 45 to 75.
“I wholeheartedly agree with this recommendation,” said Raymond N. DuBois, MD, PHD, Fellow of the AACR Academy and co-editor-in-chief of the AACR journal Cancer Prevention Research. DuBois is the dean of the College of Medicine at the Medical University of South Carolina, director of Hollings Cancer Center and an expert in cancer prevention and the biology of colorectal cancer.
Raymond N. DuBois, MD, PHD, FAACR
“Colorectal cancer is one of those cancers that has a clear-cut timeline, so if you catch it early enough you can prevent the disease or avoid regional and metastatic spread. Today, colorectal cancer is very difficult to treat when the patient presents with stage 4 disease. Avoiding advanced disease is the key to improving survival,” DuBois said.
Black adults have the highest incidence of and mortality from colorectal cancer compared to other races or ethnicities, DuBois noted.
“This recommendation will help us detect cancer in Black adults at an earlier point so that we can reduce the overall burden of colorectal cancer in the Black community,” he said.
Colorectal cancer is the second leading cause of cancer death in the United States, with 53,200 people expected to die from the disease in 2020, according to federal estimates.
“Young-onset colorectal cancer is becoming a much more serious problem in this country,” DuBois said, and the recommendation to start screening at age 45 will help pick up some of those cases.
He noted that since 1994, cases of young-onset colorectal cancer have increased by 51 percent. According to the National Cancer Institute, 11 percent of colon cancer diagnoses and 18 percent of rectal cancer diagnoses occur in individuals under the age of 50.
DuBois said lowering the recommended age for colorectal cancer screening will increase the number of people who should be screened at a time when, because of the pandemic, screening for all cancers is down.
“We just need to be diligent about encouraging everybody to get their screening when it is indicated,” he said. “Our clinics have to adapt to the reality of COVID, but it is possible to mask up, social distance, be vigilant about hygiene, and take other precautions to decrease COVID risk factors, and still have people undergo screening exams at the appropriate time.”
The task force said screening methods include stool tests, colonoscopy, CT colonography, or flexible sigmoidoscopy. Recommended screening intervals range from annually for fecal occult blood tests to every 10 years for colonoscopies.
Until the recommendation is finalized, individuals at average risk for colorectal cancer should consult their physicians to understand what screening is best for them.
DuBois said the various testing methods have their plusses and minuses, and that a positive finding on most tests has to be confirmed through a colonoscopy in order to obtain a tissue diagnosis and/or remove premalignant disease.
“Specialists always argue for their favorite test,” he said. “But any test is better than no test. Some screening is better than no screening. Ultimately, our goal is to enable all people who need cancer screening to obtain those services.”
