New Immunotherapeutic Approved for Bladder Cancer
The approval provides the first new treatment option in more than 30 years for patients with the most common type of bladder cancer
A first-of-its kind immunotherapeutic, atezolizumab (Tecentriq), was recently approved by the U.S. Food and Drug Administration (FDA) for treating certain patients with advanced bladder cancer.
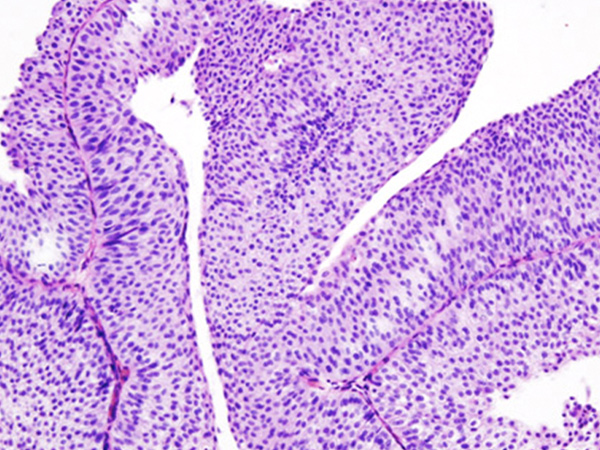
Atezolizumab is intended for patients with locally advanced or metastatic urothelial carcinoma – the most common form of bladder cancer ? whose disease has progressed during or following treatment with platinum-based chemotherapy or whose disease progressed within 12 months of platinum-based chemotherapy given before or after surgery.
Bladder cancer is the fifth most commonly diagnosed cancer in the United States. An estimated 76,960 U.S. adults will be diagnosed with bladder cancer and 16,390 people will die from the disease in 2016. Urothelial carcinoma accounts for 90 percent of all cases, according to Roche, the company that manufactures atezolizumab.
Prior to the approval of atezolizumab, there were no FDA-approved treatment for patients with metastatic urothelial carcinoma that had progressed despite platinum-based chemotherapy, and the outlook for these patients was poor, with median survival of around five to seven months.
The approval was based on results from the IMvigor 210 phase II clinical trial, which were published recently in The Lancet. In short, 15 percent of patients treated with atezolizumab had partial shrinkage or complete disappearance of their tumors. Among the 46 patients who had a response, 37 had an ongoing response for greater than or equal to 6 months and six for greater than or equal to 12 months.
Results from IMvigor 210 suggest that the benefit of atezoliumab was greatest amongst those patients whose tumor-infiltrating immune cells had the highest levels of PD-L1 protein on the surface, as assessed with the Ventana PD-L1 (SP142) Assay. Although physicians are not required to use this test before treating patients, the FDA approved the test to provide physicians with a tool to help determine which patients may benefit most from treatment with atezolizumab.
Given that the approval of atezolizumab centers on response data, rather than overall survival, nivolumab’s manufacturer is required by the FDA to conduct a randomized, phase III clinical trial to confirm that the immunotherapeutic improves survival for patients. The ongoing phase III IMvigor 211 clinical trial is designed to address this issue by comparing the ability of atezolizumab and chemotherapy to benefit patients with urothelial carcinoma that has progressed despite treatment with at least one platinum-based chemotherapy regimen.
Atezolizumab is the first in a new class of immunotherapeutics called PD-L1 inhibitors. PD-L1 is a protein that can trigger two brakes on cancer-fighting immune cells called T cells: PD-1 and B7.1. By targeting PD-L1, atezolizumab prevents this protein from triggering the PD-1 and B7.1 brakes on T cells, allowing the T cells to carry out their natural function and destroy cancer cells.
Two immunotherapeutics that release the PD-1 brake on T cells by targeting PD-1, nivolumab (Opdivo) and pembrolizumab (Keytruda), have already been approved by the FDA for treating certain patients with a variety of cancer types.
With the approval of atezolizumab, PD-1 or PD-L1 inhibitors are now FDA-approved treatment options for certain patients with six types of cancer—bladder cancer, Hodgkin lymphoma, melanoma, both the squamous and nonsquamous forms of non-small cell lung cancer, and renal cell carcinoma. With promising results reported at the AACR Annual Meeting 2016 from a phase III clinical trial testing nivolumab as a potential treatment for head and neck squamous cell carcinoma, as well as early promising results reported from a clinical trial testing atezolizumab as a potential treatment for triple-negative breast cancer, we may see more FDA approvals for PD-1? and PD-L1?targeted immunotherapeutics in the near future.
The FDA approval was rendered on May 17, 2016.
