T-cell Engager Approved for Aggressive Lung Cancer
The FDA has converted the accelerated approval of tarlatamab-dlle to a full approval for previously treated adults with extensive-stage small cell lung cancer.
The U.S. Food and Drug Administration (FDA) has granted traditional approval to tarlatamab-dlle (Imdelltra) as a treatment for adults with extensive-stage small cell lung cancer (ES-SCLC) whose disease has progressed on or after platinum-based chemotherapy.
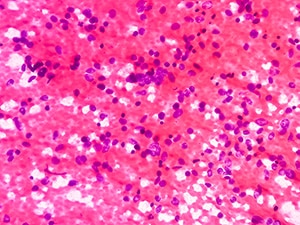
Tarlatamab-dlle is a bispecific T-cell engager, which is a type of immunotherapy that brings a patient’s T cells into close contact with cancer cells. It does so by simultaneously binding DLL3—a protein highly expressed on SCLC cells—and the CD3 protein on T cells, allowing T cells to kill DLL3-positive cells.
Tarlatamab-dlle received accelerated approval on May 16, 2024, for this indication, and is the only FDA-approved drug targeting DLL3.
The conversion to a traditional approval was based on results from the multicenter, randomized, open‑label phase III DeLLphi-304 trial, in which 509 patients with previously treated ES‑SCLC were randomly assigned (1:1) into one of two arms. One arm received tarlatamab-dlle and the other arm received one of three chemotherapy options (topotecan, lurbinectedin, or amrubicin) until progression or unacceptable toxicity. The overall survival (OS) and progression-free survival (PFS) were used to assess the efficacy of the treatment.
The median follow-up time for the tarlatamab-dlle arm and chemotherapy arm was 11.2 and 11.7 months, respectively. At the time of data collection, the median OS for patients receiving tarlatamab-dlle was 13.6 months, compared to the chemotherapy arm, which was 8.3 months. Patients treated with tarlatamab-dlle were 40% less likely to die during follow-up than those treated with chemotherapy.
Tarlatamab-dlle also delayed cancer growth—the median PFS, which is the time before the cancer became more advanced, was 4.2 months in the tarlatamab-dlle arm versus 3.2 months in the chemotherapy arm. Patients treated with tarlatamab-dlle were 28% less likely to have their cancer become more advanced or to die during the study period.
The prescribing information for tarlatamab-dlle includes a boxed warning for life-threatening or fatal cytokine release syndrome (CRS) which is caused by the rapid release of cytokines into the blood that results in symptoms like fever, nausea, headache, rash, and rapid heartbeat. The prescribing information also includes a boxed warning for neurologic toxicity, including immune effector cell-associated neurotoxicity syndrome, which is associated with increased cytokine levels in the brain and disruption of the blood-brain barrier.
The recommended dose is 1 mg on cycle 1 day 1, followed by 10 mg on days 8 and 15, and 10 mg every two weeks thereafter until disease progression or unacceptable toxicity. Tarlatamab-dlle is administered as a one-hour intravenous infusion.
SCLC is a fast-growing form of lung cancer and represents about 12% of all lung cancers. Extensive stage describes SCLC that has spread to other parts of the body. According to federal statistics, it was estimated that 226,650 individuals would be diagnosed with lung cancer and 124,730 patients would die of the disease in the United States in 2025.
The FDA rendered its decision on November 19, 2025. Check this resource for updated information on all therapeutics regulated by the FDA.