Beyond Obesity: Metabolic Health Influences Risk for Certain Cancers
Obesity is a major under-recognized contributor to the nation’s cancer toll and is quickly overtaking tobacco as the leading preventable cause of cancer.”
Ligibel et al.
Individuals who are overweight or obese are at increased risk for several types of cancer—the adenocarcinoma subtype of esophageal cancer, and colorectal, endometrial, gallbladder, kidney, pancreatic, and postmenopausal breast cancers. Overweight and obesity also negatively impact tumor recurrence, metastasis, and patient survival for some cancer types.
A major question that researchers are trying to answer is: What links obesity with cancer development and adverse survival?
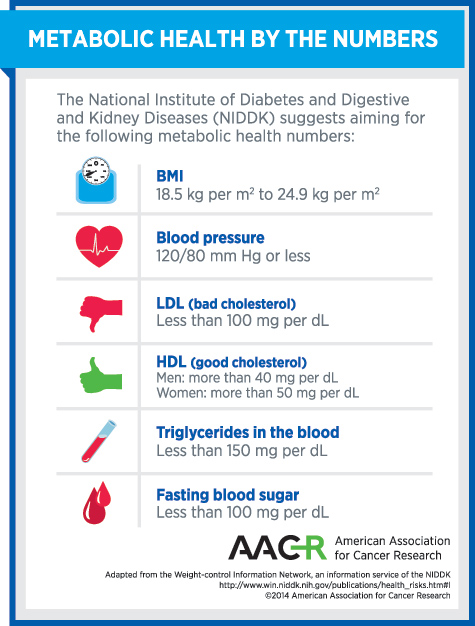
The answer to this question is complicated by the fact that most individuals who are overweight or obese have numerous other metabolic health problems, including being insulin resistant and having high blood pressure and dyslipidemia—abnormal levels of lipids such as cholesterol and triglycerides in the blood. When individuals have a combination of several metabolic health problems—including overweight/obesity, high blood pressure, high triglycerides, impaired fasting glucose, and low HDL cholesterol—at the same time, their physician may diagnose them with metabolic syndrome.
Research is beginning to reveal that the metabolic health problems often associated with overweight/obesity can themselves influence risk for certain cancers. Two studies that shed light on this were published recently in Cancer Research and Cancer Epidemiology, Biomarkers & Prevention, journals of the American Association for Cancer Research (AACR).
Poor Metabolic Health Increases Risk for Postmenopausal Breast Cancer Irrespective of Body Mass Index (BMI)
The question posed by the investigators leading the study published in Cancer Research was whether metabolic health, as measured by fasting insulin levels and the homeostatic model assessment (HOMA-IR) method for quantifying insulin resistance, would be an indicator of breast cancer risk in both women who were normal weight and those who were overweight/obese.
The researchers analyzed insulin resistance and BMI data from 3327 nondiabetic women enrolled in the Women’s Health Initiative. Among this subcohort of women, 497 received a breast cancer diagnosis over a mean of 8.2 years of follow-up.
The team found that women who were overweight and insulin resistant had an 84 percent greater risk of breast cancer than did women who were overweight but not insulin resistant. Similarly, breast cancer risk was more than double among those who were overweight and had high fasting insulin levels compared with those who were overweight but had normal fasting insulin levels.
Among women who were normal weight, breast cancer risk was twofold greater for those who had high fasting insulin levels, compared with those who had normal fasting insulin levels.
“Our data suggest that insulin resistance may be a significant factor in the development of breast cancer, irrespective of whether a woman is overweight or normal weight,” said the first author of the study, Marc J. Gunter, PhD, associate professor of cancer epidemiology and prevention in the Department of Epidemiology and Biostatistics at Imperial College London’s School of Public Health.
Metabolic Syndrome Increases Endometrial Cancer Risk Independent of Overweight/Obesity
The study published in Cancer Epidemiology, Biomarkers & Prevention focused on the role of individual metabolic health problems and risk for endometrial cancer, which is strongly linked to overweight/obesity.
The researchers used data from the SEER-Medicare linked database, which provided them with information on endometrial cancer and metabolic health, to investigate whether metabolic syndrome components other than overweight/obesity are associated with increased endometrial cancer risk.
After analyzing data from 16,323 women diagnosed with endometrial cancer between 1993 and 2007 and 100,751 controls, the team found that each distinct metabolic syndrome condition—overweight/obesity, high blood pressure, high triglycerides, and impaired fasting glucose—increased risk for endometrial cancer individually.
In addition, metabolic syndrome—as defined by U.S. National Cholesterol Education Program Adult Treatment Panel III criteria and the International Diabetes Foundation—increased endometrial cancer risk by 39 percent and 103 percent, respectively. After taking into account if a woman was overweight/obese, the increased endometrial cancer risks were 21 percent and 17 percent for the two metabolic syndrome definitions, respectively.
“We found that a diagnosis of metabolic syndrome was associated with higher risk of endometrial cancer, and that metabolic syndrome appeared to increase risk regardless of whether the woman was considered obese,” said the first author on the study, Britton Trabert, PhD, an investigator in the Division of Cancer Epidemiology and Genetics of the National Cancer Institute in Bethesda, Maryland.
The Bottom Line: Healthy Living Can Prevent Cancer
Given that overweight/obesity is considered to be quickly overtaking tobacco as the leading preventable cause of cancer, it has been clear for some time that maintaining a healthy weight and keeping active could reduce the burden of cancer. The accumulating evidence that the metabolic health problems associated with overweight/obesity can increase risk for certain cancers regardless of whether an individual is overweight or obese does nothing to diminish this idea because the best way to remain metabolically healthy is to maintain a normal-weight BMI throughout life and take regular physical exercise.