New Research Shows Promising Approaches for Brain Cancer Detection and Treatment
You’re working away on your latest project when your stomach suddenly growls. Stepping away from your desk, you head to the kitchen and, after a few minutes of deliberation, finally decide on a sandwich. The salty meats, crisp lettuce, and soft bread, washed down with a tall glass of cold iced tea, are exactly what you needed. Satisfied, you return to work as your body begins to digest the meal.
A mundane, seemingly unremarkable series of events like this is so routine that we seldom consider the multitude of processes involved in making it happen. Decision-making, motor skills, senses like taste and touch, and involuntary actions such as digestion and breathing—all these diverse processes play a role in our everyday lives and are controlled by the brain, the most complex organ in the human body.
It’s no surprise, then, that diseases affecting the brain, including cancer, can have devastating consequences for a patient’s quality of life and life expectancy. Patients with brain cancer face a grim prognosis—on average, fewer than one-third of patients are expected to survive five years past diagnosis, and the outlook can be even worse for patients with particularly lethal types of brain cancer.
Several factors contribute to the high mortality rates of brain cancer, including the aggressive nature of the disease and impediments to treatment. Ironically, the very features that protect the brain can impair the efficacy of certain treatments. The blood-brain barrier, for example, is critical for keeping toxins and pathogens out of the brain, but it is also an obstacle for various cancer therapies. Chemotherapy and radiation therapy are stalwarts in cancer treatment; however, the use of these toxic therapies must be limited in the brain to prevent brain damage. While other cancer types, including breast and prostate cancers, can be treated by complete resection of the diseased site, resection of large areas of the brain is not an option.
Despite these challenges, ongoing research continues to move the field forward. Here, we highlight some of the latest advances in early detection and treatment for brain cancer.
A liquid biopsy-based test for the early detection of brain tumors
The early diagnosis of cancer is crucial to preventing delays in treatment, but the nonspecific symptoms associated with brain cancer can make it difficult to distinguish between patients with brain cancer and those with less serious conditions. To facilitate diagnosis, researchers have developed an early detection test that can identify signs of brain cancer just by analyzing a patient’s blood sample, a technique known as liquid biopsy. The test, called BRAIN-ED, was recently evaluated in 1,004 patients who had symptoms potentially indicative of brain cancer.
In this study, BRAIN-ED accurately identified 81 percent of individuals with a brain tumor, including 91 percent of patients with glioblastoma, the most common and aggressive type of brain cancer. The test also correctly identified 80 percent of individuals who did not have a brain tumor.
Liquid biopsy-based tests such as BRAIN-ED are an exciting new direction in cancer research. Several other liquid biopsy-based early detection tests were presented at the AACR Annual Meeting 2021 and were discussed in a recent blog post.
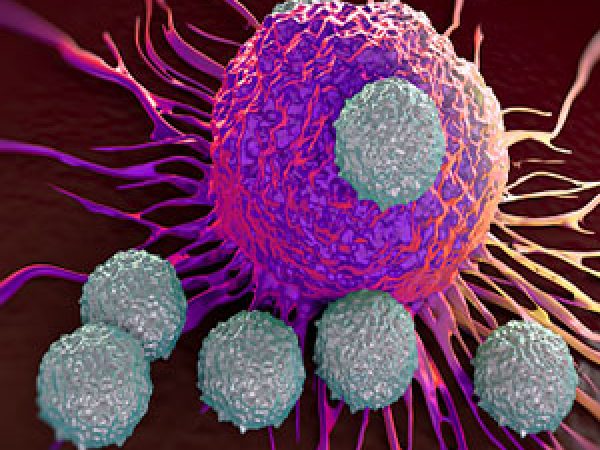
New strategies to improve immunotherapy responses
While immunotherapies have revolutionized treatment for many cancer types, they have thus far been relatively unsuccessful in brain cancer. In addition to the blood-brain barrier, which can prevent immunotherapies from reaching the brain, an immunosuppressive tumor microenvironment allows brain tumors to evade antitumor immune responses. Research continues to identify potential ways to improve immunotherapy responses in patients with brain cancer.
An oncolytic virus shows promise for treating pediatric brain cancer
A new immunotherapy approach took advantage of the ability of herpesviruses—common causes of cold sores—to infect neuronal cells, thereby avoiding the blood-brain barrier and gaining access to the brain. By removing the genes needed by the virus to evade antiviral defenses in healthy cells, researchers developed a virus that would selectively infect and kill brain cancer cells—where many antiviral pathways are already inactive—while leaving normal cells alone.
Results of a phase I clinical trial testing this immunotherapy in pediatric patients were presented at the Annual Meeting and described in a recent blog post. Briefly, researchers found that the engineered virus was well tolerated and led to longer survival and greater antitumor immune responses than would be expected for this disease, highlighting a potential new immunotherapy strategy for brain cancers.
Understanding immune evasion in glioblastoma
Identifying additional factors that impair antitumor immune responses may help uncover new strategies to improve clinical outcomes in patients receiving immunotherapy.
Two studies recently published in Cell identified molecular mechanisms underlying immune evasion in glioblastoma. By sequencing T cells that infiltrated brain tumors, the researchers of one study identified the CD161 cell surface protein as a potential inhibitor of antitumor immune responses. Further experimentation in cell and animal models of glioblastoma confirmed the role of CD161 in immune evasion, raising the possibility of therapeutically targeting CD161 to boost antitumor immunity. The second study found that glioblastoma stem cells undergo epigenetic remodeling upon immune attack that results in changes in gene expression and the recruitment of immunosuppressive proteins. The genes and pathways activated by such epigenetic remodeling may present potential therapeutic opportunities.
In addition to biological factors, other drugs in a patient’s treatment regimen may also influence responses to immunotherapy. Patients with glioblastoma are commonly treated with a steroid called dexamethasone to help reduce the risk of cerebral edema, but recent data suggests that this otherwise beneficial treatment may impair the efficacy of immunotherapy. The retrospective analysis, published in the AACR journal Clinical Cancer Research and highlighted in an AACR press release, found that patients with glioblastoma who had been treated with immunotherapy and dexamethasone had twice the risk of death as those treated with immunotherapy alone, even after adjusting for patient and tumor characteristics. Based on these findings, the researchers suggest omitting dexamethasone treatment in patients receiving immunotherapy as a way to potentially improve clinical outcomes.
While brain cancer remains fatal for most patients, new research continues to reveal promising new avenues to improve the diagnosis and treatment of this terrible disease.