Editors’ Picks: April Highlights from AACR Journals
Earlier this month, over 21,000 researchers, clinicians, patients, and other stakeholders gathered at the AACR Annual Meeting 2023 to discuss the latest advances across the continuum of cancer research—from basic science to clinical research to epidemiology.
Like its meetings, the AACR journals also span the breadth of cancer research, and this month, the editors of the 10 AACR journals have spotlighted results from four clinical trials, an analysis on the contributions of race and socioeconomic status to disparities in head and neck cancer, and mechanistic insights into immune evasion gleaned from preclinical models, among other studies.
The abstracts of the featured articles are included below. For complete details, follow the links to the full-text articles, which are freely available for a limited time.
Journal: Cancer Research Communications
Vitamin D deficiency is associated with an increased risk of prostate cancer mortality and is hypothesized to contribute to prostate cancer aggressiveness and disparities in African American populations. The prostate epithelium was recently shown to express megalin, an endocytic receptor that internalizes circulating globulin-bound hormones, which suggests regulation of intracellular prostate hormone levels. This contrasts with passive diffusion of hormones that is posited by the free hormone hypothesis. Here, we demonstrate that megalin imports testosterone bound to sex hormone-binding globulin into prostate cells. Prostatic loss of Lrp2 (megalin) in a mouse model resulted in reduced prostate testosterone and dihydrotestosterone levels. Megalin expression was regulated and suppressed by 25-hydroxyvitamin D (25D) in cell lines, patient-derived prostate epithelial cells, and prostate tissue explants. In patients, the relationships between hormones support this regulatory mechanism, as prostatic DHT levels are higher in African American men and are inversely correlated with serum 25D status. Megalin levels are reduced in localized prostate cancer by Gleason grade. Our findings suggest that the free hormone hypothesis should be revisited for testosterone and highlight the impact of vitamin D deficiency on prostate androgen levels, which is a known driver of prostate cancer. Thus, we revealed a mechanistic link between vitamin D and prostate cancer disparities observed in African Americans.
Journal: Blood Cancer Discovery

We conducted a phase I clinical trial of anti-BCMA chimeric antigen receptor T cells (CART-BCMA) with or without anti-CD19 CAR T cells (huCART19) in multiple myeloma (MM) patients responding to third- or later-line therapy (phase A, N = 10) or high-risk patients responding to first-line therapy (phase B, N = 20), followed by early lenalidomide or pomalidomide maintenance. We observed no high-grade cytokine release syndrome (CRS) and only one instance of low-grade neurologic toxicity. Among 15 subjects with measurable disease, 10 exhibited partial response (PR) or better; among 26 subjects responding to prior therapy, 9 improved their response category and 4 converted to minimal residual disease (MRD)–negative complete response/stringent complete response. Early maintenance therapy was safe, feasible, and coincided in some patients with CAR T-cell reexpansion and late-onset, durable clinical response. Outcomes with CART-BCMA + huCART19 were similar to CART-BCMA alone. Collectively, our results demonstrate favorable safety, pharmacokinetics, and antimyeloma activity of dual-target CAR T-cell therapy in early lines of MM treatment.
This article was highlighted and featured on the cover of the most recent issue.
Journal: Cancer Discovery
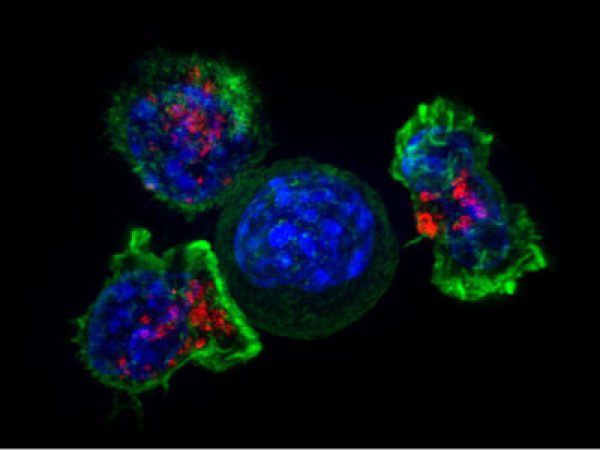
Glioblastoma (GBM) constitutes the most lethal primary brain tumor for which immunotherapy has provided limited benefit. The unique brain immune landscape is reflected in a complex tumor immune microenvironment (TIME) in GBM. Here, single-cell sequencing of the GBM TIME revealed that microglia were under severe oxidative stress, which induced nuclear receptor subfamily 4 group A member 2 (NR4A2)–dependent transcriptional activity in microglia. Heterozygous Nr4a2 (Nr4a2+/−) or CX3CR1+ myeloid cell–specific Nr4a2 (Nr4a2fl/flCx3cr1Cre) genetic targeting reshaped microglia plasticity in vivo by reducing alternatively activated microglia and enhancing antigen presentation capacity for CD8+ T cells in GBM. In microglia, NR4A2 activated squalene monooxygenase (SQLE) to dysregulate cholesterol homeostasis. Pharmacologic NR4A2 inhibition attenuated the protumorigenic TIME, and targeting the NR4A2 or SQLE enhanced the therapeutic efficacy of immune-checkpoint blockade in vivo. Collectively, oxidative stress promotes tumor growth through NR4A2–SQLE activity in microglia, informing novel immune therapy paradigms in brain cancer.
This article is highlighted and featured on the cover of the April issue.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Background: Head and neck cancer (HNC) mortality differs by race, ethnicity, and socioeconomic status (SES). However, it is unclear whether the relationship between race/ethnicity and HNC-specific mortality varies according to the residence-level SES. Methods: Data from the Surveillance Epidemiology and End Results database included participants with primary HNC between 2006 and 2017 (followed through 2018) to assess the joint association of race/ethnicity and census-tract level SES Yost-index groups (quintiles) with all-cause and HNC-specific mortalities. Relative survival rates at 1, 5, and 10 years were calculated. Multivariable Cox proportional hazard regression models estimated hazard-ratios and 95% confidence intervals for all-cause mortality, and Fine-Gray subdistribution hazard models for HNC-specific mortality. Cumulative incidence curves for HNC-specific deaths were estimated. Results: 76,095 patients were included in the analysis: 63.2% were <65 years, 73.4% male, and 11.3% non-Hispanic (NH) Black. Most patients (58.3%) were diagnosed at regional or distant stages and 20.6% died of HNC. The five-year relative survival rate increased with SES group, with 51.6% in the lowest SES group, and 74.1% in the highest SES group. NH-Black patients had higher risk of all-cause and HNC-specific mortality than NH-White patients, regardless of the SES group. NH-Asian/Pacific Islander and Hispanic patients had higher risk of HNC-specific mortality in some SES groups. Conclusions: NH-Black patients of all SES strata had significantly worse outcomes. Other factors, such as healthcare quality, may be associated with persistent disparities. Impact: The study highlights the persistence of significant racial disparities in HNC survival across socioeconomic categories. There is need to consider additional factors underlying these disparities.
This article is highlighted in the April issue.
Journal: Cancer Immunology Research
Intratumoral cytotoxic CD8+ T cells (CTL) enter a dysfunctional state characterized by expression of coinhibitory receptors, loss of effector function, and changes in the transcriptional landscape. Even though several regulators of T-cell exhaustion have been identified, the molecular mechanisms inducing T-cell exhaustion remain unclear. Here, we show that IL18 receptor (IL18R) signaling induces CD8+ T-cell exhaustion in a murine pancreatic cancer model. Adoptive transfer of Il18r−/− OT-1 CD8+ CTLs resulted in enhanced rejection of subcutaneous tumors expressing ovalbumin (OVA) as a model antigen (PancOVA), compared with wild-type OT-1 CTLs. Transferred intratumoral IL18R-deficient CTLs expressed higher levels of effector cytokines TNF and IFNγ and had reduced expression of coinhibitory receptors (PD-1, TIM-3, 2B4, LAG-3) and the transcription factors Eomes and TOX. Lower expression of coinhibitory receptors and TOX on IL18R-deficient versus IL18R-sufficient CD8+ T cells were confirmed in an orthotopic KPC model. IL18R-induced T-cell exhaustion was regulated by IL2/STAT5 and AKT/mTOR pathways, as demonstrated in an in vitro exhaustion assay. Concordantly, mice deficient in NLRP3, the molecular complex activating IL18, had decreased expression of coinhibitory receptors on intratumoral T cells and similar changes in signaling pathways at the transcriptome level. Thus, molecular pathways promoting T-cell exhaustion indicate an involvement of an NLRP3-expressing tumor microenvironment, which mediates IL18 release. The Cancer Genome Atlas analysis of patients with pancreatic carcinoma showed an association between NLRP3-mediated IL18 signaling and shorter survival. These findings indicate NLRP3-mediated IL18R signaling as a regulator of intratumoral T-cell exhaustion and a possible target for immunotherapy.
A related commentary can be found here.
Journal: Cancer Prevention Research
Patients with human papillomavirus type 16 (HPV16) infection and low-grade cervical dysplasia [low-grade squamous intraepithelial lesion (LSIL)/CIN1] or atypical squamous cells [atypical squamous cells of undetermined significance (ASC-US)/atypical squamous cells- cannot exclude high-grade squamous intraepithelial lesion (ASC-H)] require active surveillance for disease progression. A safe and effective immunotherapy to clear HPV16 is an unmet medical need. The safety run-in cohort of a randomized double-blind, placebo-controlled phase II trial of PVX2 [vaccination twice with HPV16-targeting pNGVL4a-Sig/E7(detox)/HSP70 plasmid and once with the HPV16 L2E7E6 fusion protein “TA-CIN”] as immunotherapy for patients with HPV16+ ASC-US, ASC-H, or LSIL/CIN1 (NCT03911076) was recently completed. The primary objective of this cohort was to determine the safety and tolerability of PVX2 vaccination. Subjects were confirmed to have HPV16 infection and LSIL/CIN1, ASC-US, or ASC-H. Adverse events were evaluated using Common Terminology Criteria for Adverse Events v5.0. HPV typing by HPV16 18/45 Aptima Assay was done at baseline, month 6, and month 12, with simultaneous cytology analysis. Cervical biopsies and endocervical curettage were performed at baseline and month 6. In the safety run-in cohort 12 eligible patients were enrolled. Each received three monthly immunizations. One was lost to follow-up after week 12. There were no serious adverse events. A total of five adverse events were noted by 4 patients; 4 were considered not vaccine-related, and one ‘unlikely related’ by the investigator. At month 6, 45% (5/11) of participants converted to HPV16-negative and 2 others developed CIN2+ and received a loop electrosurgical excision procedure. At month 12, 64% (7/11) were HPV16-negative, including those HPV16-negative at month 6. In conclusion, PVX2 immunotherapy was well tolerated and associated with viral regression, supporting further testing.
This article is featured on the cover of the April issue.
Journal: Cancer Research (April 1st issue)
The microenvironment that surrounds pancreatic ductal adenocarcinoma (PDAC) is profoundly desmoplastic and immunosuppressive. Understanding triggers of immunosuppression during the process of pancreatic tumorigenesis would aid in establishing targets for effective prevention and therapy. Here, we interrogated differential molecular mechanisms dependent on cell of origin and subtype that promote immunosuppression during PDAC initiation and in established tumors. Transcriptomic analysis of cell-of-origin–dependent epithelial gene signatures revealed that Nt5e/CD73, a cell-surface enzyme required for extracellular adenosine generation, is one of the top 10% of genes overexpressed in murine tumors arising from the ductal pancreatic epithelium as opposed to those rising from acinar cells. These findings were confirmed by IHC and high-performance liquid chromatography. Analysis in human PDAC subtypes indicated that high Nt5e in murine ductal PDAC models overlaps with high NT5E in human PDAC squamous and basal subtypes, considered to have the highest immunosuppression and worst prognosis. Multiplex immunofluorescent analysis showed that activated CD8+ T cells in the PDAC tumor microenvironment express high levels of CD73, indicating an opportunity for immunotherapeutic targeting. Delivery of CD73 small-molecule inhibitors through various delivery routes reduced tumor development and growth in genetically engineered and syngeneic mouse models. In addition, the adenosine receptor Adora2b was a determinant of adenosine-mediated immunosuppression in PDAC. These findings highlight a molecular trigger of the immunosuppressive PDAC microenvironment elevated in the ductal cell of origin, linking biology with subtype classification, critical components for PDAC immunoprevention and personalized approaches for immunotherapeutic intervention.
A related commentary can be found here.
Journal: Cancer Research (April 15th issue)
Crossing the blood–brain barrier is a crucial, rate-limiting step of brain metastasis. Understanding of the mechanisms of cancer cell extravasation from brain microcapillaries is limited as the underlying cellular and molecular processes cannot be adequately investigated using in vitro models and endpoint in vivo experiments. Using ultrastructural and functional imaging, we demonstrate that dynamic changes of activated brain microcapillaries promote the mandatory first steps of brain colonization. Successful extravasation of arrested cancer cells occurred when adjacent capillary endothelial cells (EC) entered into a distinct remodeling process. After extravasation, capillary loops were formed, which was characteristic of aggressive metastatic growth. Upon cancer cell arrest in brain microcapillaries, matrix-metalloprotease 9 (MMP9) was expressed. Inhibition of MMP2/9 and genetic perturbation of MMP9 in cancer cells, but not the host, reduced EC projections, extravasation, and brain metastasis outgrowth. These findings establish an active role of ECs in the process of cancer cell extravasation, facilitated by cross-talk between the two cell types. This extends our understanding of how host cells can contribute to brain metastasis formation and how to prevent it.
A related commentary can be found here.
Journal: Clinical Cancer Research (April 1st issue)
Randomized Phase II Trial of Sunitinib or Cediranib in Alveolar Soft Part Sarcoma
Purpose: Alveolar soft part sarcoma (ASPS) is a rare, highly vascular tumor with few treatment options. We designed a phase II randomized trial to determine the activity and tolerability of single-agent cediranib or sunitinib in patients with advanced metastatic ASPS. Patients and Methods: Patients 16 years of age and older were randomized to receive cediranib (30 mg) or sunitinib (37.5 mg) in 28-day cycles. Patients could cross over to the other treatment arm at disease progression. The primary endpoint was to measure the objective response rate (ORR) for each agent. Median progression-free survival (mPFS) for the two arms was also determined. Results: Twenty-nine of 34 enrolled patients were evaluable for response. One patient on each of the initial two treatment arms had a partial response (ORR: 6.7% and 7.1% for cediranib and sunitinib, respectively). Twenty-four patients had a best response of stable disease (86.7% and 78.6% for cediranib and sunitinib, respectively). There were no significant differences in mPFS for the two treatment arms. Clinical benefit (i.e., objective response or stable disease for a minimum of four or six cycles of therapy) on the first-line tyrosine kinase inhibitor (TKI) therapy did not predict benefit on the second-line TKI. Both drugs were well tolerated. As of August 2021, 1 patient (unevaluable for ORR) remains on study. Conclusions: The study did not meet its endpoints for ORR. Although both TKIs provided clinical benefit, the outcomes may have been attenuated in patients who had progressed ≤6 months before enrollment, potentially accounting for the low response rates.
This article is highlighted in the April 1st issue. A related commentary can be found here.
Journal: Clinical Cancer Research (April 15th issue)
Purpose: To investigate the efficacy and safety of the novel orally active PI3Kδ inhibitor in relapsed and/or refractory patients with follicular lymphoma (FL) who had received at least two prior systemic treatments. Patients and Methods: Histologically confirmed relapsed and/or refractory patients with FL with disease progression after receiving second-line or greater systemic therapy were enrolled. Linperlisib was administered at 80 mg every day, orally in a 28-day cycle until disease progression or intolerable toxicity occurred. The primary outcome for the study was the objective response rate (ORR), with secondary outcomes including the duration of response (DOR), progression-free survival (PFS), overall survival (OS), disease control rate, and drug safety profile. Results: Of 114 screened relapsed and/or refractory patients with FL, 84 were enrolled in the full analysis set (FAS). The ORR of the 84 FAS patients was 79.8% [95% confidence interval (CI), 69.6–87.8, 67 patients], with 13 patients (15.5%) achieving a complete response and 54 patients (64.3%) with a partial response. The median DOR was 12.3 months (95% CI, 9.3–15.9). The median PFS was 13.4 months (95% CI, 11.1–16.7). The 12-month OS rate was 91.4% (95% CI, 82.7–95.8) and a median OS not reached by 42 months. The most frequent (>3%) treatment-related adverse events Grade ≥3 were infectious pneumonia (19.0%), neutropenia (15.5%), decreased lymphocyte count (4.8%), decreased leukocyte count (4.8%), increased lipase (3.6%), decreased platelet count (3.6%), hypertriglyceridemia (3.6%), and interstitial lung disease (3.6%). Conclusions: Linperlisib demonstrated compelling clinical activity and manageable tolerability for relapsed and/or refractory patients with FL who had received at least two prior systemic therapies.
This article is highlighted in the April 15th issue.
Journal: Molecular Cancer Research
Cancer cells undergo metabolic reprogramming to meet increased bioenergetic demands. Studies in cells and mice have highlighted the importance of oxidative metabolism and lipogenesis in prostate cancer; however, the metabolic landscape of human prostate cancer remains unclear. To address this knowledge gap, we performed radiometric (14C) and stable (13C) isotope tracing assays in precision-cut slices of patient-derived xenografts (PDX). Glucose, glutamine, and fatty acid oxidation was variably upregulated in malignant PDXs compared with benign PDXs. De novo lipogenesis (DNL) and storage of free fatty acids into phospholipids and triacylglycerols were increased in malignant PDXs. There was no difference in substrate utilization between localized and metastatic PDXs and hierarchical clustering revealed marked metabolic heterogeneity across all PDXs. Mechanistically, glucose utilization was mediated by acetyl-CoA production rather than carboxylation of pyruvate, while glutamine entered the tricarboxylic acid cycle through transaminase reactions before being utilized via oxidative or reductive pathways. Blocking fatty acid uptake or fatty acid oxidation with pharmacologic inhibitors was sufficient to reduce cell viability in PDX-derived organoids, whereas blockade of DNL, or glucose or glutamine oxidation induced variable and limited therapeutic efficacy. These findings demonstrate that human prostate cancer, irrespective of disease stage, can effectively utilize all metabolic substrates, albeit with marked heterogeneity across tumors. We also confirm that fatty acid uptake and oxidation are targetable metabolic dependencies in human prostate cancer.
This article is highlighted in the April issue.
Journal: Molecular Cancer Therapeutics
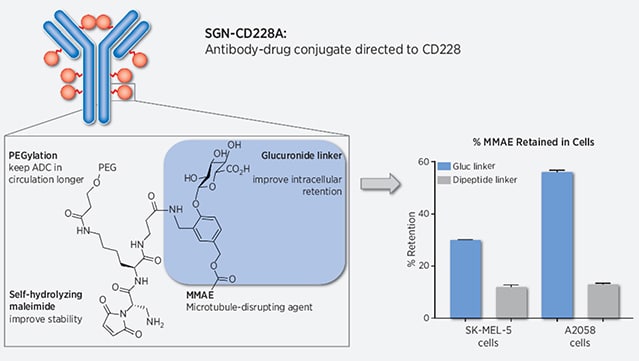
SGN-CD228A Is an Investigational CD228-Directed Antibody–Drug Conjugate with Potent Antitumor Activity across a Wide Spectrum of Preclinical Solid Tumor Models
SGN-CD228A is an investigational antibody–drug conjugate (ADC) directed to melanotransferrin (CD228, MELTF, MFI2, p97), a cell-surface protein first identified in melanoma. SGN-CD228A consists of a humanized antibody, hL49, with high specificity and affinity for CD228 that is stably conjugated to 8 molecules of the clinically validated microtubule-disrupting agent monomethyl auristatin E (MMAE) via a novel glucuronide linker. We performed comprehensive IHC studies, which corroborated published RNA sequencing data and confirmed low CD228 expression in normal tissues and high expression in several cancers, including melanoma, squamous non–small cell lung cancer (NSCLC), triple-negative breast cancer (TNBC), colorectal cancer, and pancreatic cancer. SGN-CD228A was efficiently internalized in various tumor cell types, and its cytotoxic activity was dependent on CD228 expression and internalization and intrinsic sensitivity to the MMAE payload. Compared with the valine-citrulline dipeptide linker, the novel glucuronide linker increased the cellular retention of MMAE in vitro and conferred improved antitumor activity against melanoma cell lines in vitro and in vivo. In addition, SGN-CD228A was active across melanoma, TNBC, and NSCLC cell line- and patient-derived xenograft models with heterogeneous antigen expression. In vivo, CD228 expression was important for response to SGN-CD228A but was not well correlated across all tumor types, suggesting that other factors associated with ADC activity are important. Overall, SGN-CD228A is a CD228-directed, investigational ADC that employs innovative technology and has compelling preclinical antitumor activity. SGN-CD228A is investigated in a Phase I clinical trial (NCT04042480) in patients with advanced solid tumors.
This article is highlighted in the April issue.