Identifying Breast Cancer Patients Likely to Respond to Chemotherapy
Using whole-genome sequencing, researchers have found mutational patterns that may identify breast cancer patients most likely to benefit from certain types of chemotherapy.
Breast cancer is the most commonly diagnosed cancer among women living in the United States, according to statistics from the National Cancer Institute.
“Many patients with breast cancer, especially those with the difficult-to-treat triple-negative subtype, are treated with platinum-based chemotherapies like cisplatin, but not all have responses to this treatment,” said Steven J.M. Jones, PhD, the lead author of a study recently published in Clinical Cancer Research, a journal of the American Association for Cancer Research.
In the study, Dr. Jones, who is head of bioinformatics and codirector of Canada’s Michael Smith Genome Sciences Centre at BC Cancer in Vancouver, British Columbia, and his colleagues found that whole-genome sequencing of breast cancers can reveal mutational patterns that identify patients who are likely to respond well to platinum-based chemotherapies.
“As whole-genome sequencing becomes more affordable, this presents an opportunity to improve breast cancer treatment,” Dr. Jones said.
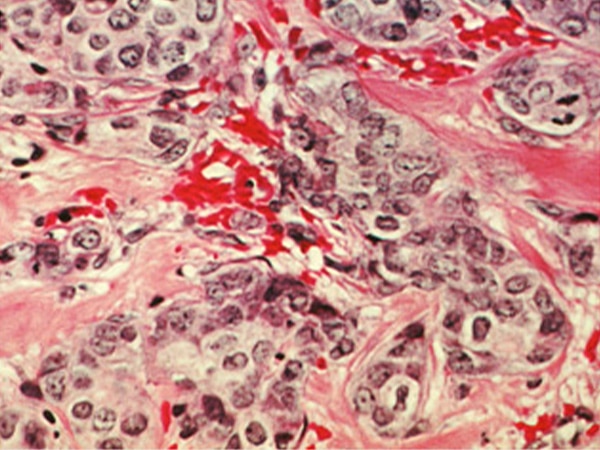
Platinum-based chemotherapies are chemicals containing the heavy metal platinum. They attach to DNA, interfering with normal cellular process that are vital for cancer cell proliferation and survival, and ultimately causing the cancer cells to die.
Platinum-based chemotherapy is particularly effective for the 5 to 10 percent of patients with breast cancer whose tumors have hereditary BRCA1 and BRCA2 mutations. These cancers have deficiencies in a cellular process called homologous recombination, which is involved in repairing damaged DNA.
Hereditary BRCA1 and BRCA2 mutations are not the only cause of homologous recombination deficiency. In fact, genomic mutational signatures that are characteristic of homologous recombination deficiency are found in as many as 20 to 40 percent of breast cancers, according to Dr. Jones.
Eric Y. Zhao, a graduate student in Jones’ laboratory; and colleagues, therefore, set out to determine whether genomic mutational patterns characteristic of homologous recombination deficiency are associated with good responses to platinum-based chemotherapy.
The researchers performed whole-genome sequencing on tumor tissue and matched normal tissue from 93 patients with breast cancer, 33 of whom had been treated with a platinum-based chemotherapy. After analyzing the data for the presence of six mutational signatures associated with homologous recombination deficiency, they used a mathematical model called HRDetect, previously shown to predict BRCA1 and BRCA2 deficiency, to calculate an HRDetect score for each breast cancer.
Nineteen breast cancers had high HRDetect scores (greater than 0.7), 37 had moderate scores (0.005-0.7), and 37 had low scores (less than 0.005).
Further analysis showed that after adjusting for BRCA1/2 mutation status, high HRDetect scores were significantly associated with clinical improvement, as assessed by radiographic tumor shrinkage, following platinum-based chemotherapy. Among the 26 patients who had been treated with a platinum-based chemotherapy and for whom imaging data were available, clinical improvement was observed for eight of the 11 patients whose breast cancers had high HRDetect scores but only two of the 15 patients whose breast cancers had moderate or low HRDetect scores.
The median total duration on platinum-based chemotherapy and median overall survival was 3 months and 1.3 years longer, respectively, for those with high HRDetect scores compared with those with low HRDetect scores. However, the researchers cautioned that these results should be interpreted carefully as they were calculated based on data from a small number of patients.
According to Dr. Jones, the main limitation of the study is that it was observational, meaning that the researchers examined a patient cohort for a clinically meaningful correlation, and that it, therefore, does not establish causation. He explained that establishing causation would require a randomized controlled trial but that the findings of their study will likely be helpful in the design of such a trial.
This study was supported by funds from the BC Cancer Foundation. Contributions toward equipment and infrastructure came from the Canada Foundation for Innovation and the BC Knowledge Development Fund.
