AACR Virtual Annual Meeting I: The Promises and Challenges of Expanding the Use of Immune Checkpoint Inhibitors Through Combination Therapy
The cutting-edge scientific program for the AACR Virtual Annual Meeting I began Monday, April 27, with an Opening Clinical Plenary featuring results from four high-impact clinical trials. Session chairperson Nilofer S. Azad, MD, explained in her introductory remarks that the organizers hope that the clinical trial presentations will provide a beacon of hope to cancer patients during the COVID-19 pandemic, highlighting how researchers are still on a mission to drive progress against the devastating collection of diseases called cancer. Azad, who is associate professor of oncology at Johns Hopkins University School of Medicine, was also cochair of the Clinical Trials Committee for the terminated AACR Annual Meeting 2020.

The use of immunotherapeutics called immune checkpoint inhibitors as treatments for cancer has expanded dramatically in the past five years. During that time, the number of immune checkpoint inhibitors approved by the U.S. Food and Drug Administration (FDA) has increased from three to seven. In addition, the number of types of cancer that can be treated by one or more of these revolutionary anticancer therapeutics has increased from two to 16. One immune checkpoint inhibitor is also approved for treating any type of solid tumor that tests positive for either of two specific biomarkers, microsatellite instability–high or mismatch repair–deficiency.
The excitement surrounding immune checkpoint inhibitors stems from the fact that they yield unprecedented long-term responses across a wide array of cancer types. However, not all patients respond to immune checkpoint inhibitor treatment. Moreover, some patients whose tumors respond initially to such treatment eventually relapse because their tumors become treatment-resistant. One approach that researchers are testing to try and increase the number of patients who benefit from immune checkpoint inhibitors is combining these immunotherapeutics with therapeutics that target other molecular drivers of tumor growth.
Three of the clinical trials presented in the Opening Clinical Plenary investigated the use of an immune checkpoint inhibitor in combination with molecularly targeted therapy. Here, we discuss one trial of a promising immunotherapy–targeted therapy combination for breast cancer and one trial that highlights the challenges of this approach in the treatment of prostate cancer. The third immune checkpoint inhibitor trial in the session is covered in a separate post highlighting progress against melanoma.
The Promise: Combining Immune Checkpoint Inhibitor and PARP Inhibitor Therapy for Breast Cancer
Breast cancer is the most commonly diagnosed cancer among U.S. women, and it is the second most common cause of cancer death for this group. Outcomes vary widely depending on the type of breast cancer a women is diagnosed with, according to the National Cancer Institute (NCI). Those who have breast cancer lacking the protein HER2 (HER2-negative breast cancer) have poorer outcomes than those who have HER2-positive breast cancer. Among those who have HER2-negative breast cancer, outcomes are far worse for those whose cancer also lacks hormone receptors (HR-negative, HER2-negative breast cancer; often called triple-negative breast cancer). For example, the five-year relative survival rate for regional, HR-negative, HER2-negative breast is 65 percent, compared with 90 percent for regional, HR-positive, HER2-negative breast cancer.
A landmark in the treatment of HER2-negative breast cancer was the March 2019 FDA approval of the PDL1-targeted immune checkpoint inhibitor atezolizumab (Tecentriq) for use in combination with the cytotoxic chemotherapeutic nab-paclitaxel (Abraxane) to treat adults who have unresectable locally advanced or metastatic triple-negative breast cancer that expresses the protein PDL1. As of the start of the AACR Virtual Annual Meeting I, this remained the only approval for using immune checkpoint inhibitors in the treatment of breast cancer, but there were many clinical trials underway looking to build on this milestone approval.
In the first presentation in the Opening Clinical Plenary, Lajos Pusztai, MD, DPhil, from Yale University in New Haven, Connecticut, reported results from the arm of the I-SPY-2 clinical trial in which the researchers tested whether adding the immune checkpoint inhibitor durvalumab (Imfinzi) and the targeted therapeutic olaparib (Lynparza) to standard neoadjuvant (presurgery) chemotherapy improved outcomes for women with stage II/III, HER2-negative breast cancer. Olaparib targets PARP proteins; it was approved by the FDA for treating metastatic, HER2-negative breast cancer patients who have an inherited BRCA1/2 mutation in January 2018.

Pusztai explained that the I-SPY-2 clinical trial is a platform clinical trial with multiple concurrent experimental arms and a shared standard cytotoxic chemotherapy control arm comprising infusions of paclitaxel once a week for 12 weeks followed by four courses of anthracycline-based chemotherapy. The treatments are given presurgery and the primary outcome being assessed is whether the experimental treatments increase the proportion of patients who have a pathologic complete response (pCR), which the researchers defined as no residual invasive cancer detected in breast tissue and lymph nodes removed during surgery.
There were 73 patients with HER2-negative breast cancer enrolled in the arm of the I-SPY-2 clinical trial discussed by Pusztai, but only 72 completed surgery and were evaluable for pCR. The researchers found that adding durvalumab and olaparib to paclitaxel significantly improved the pCR rate for patients with HER2-negative breast cancer compared with standard cytotoxic chemotherapy. The estimated pCR rates for patients with HER2-negative breast cancer were 37 percent for those receiving durvalumab, olaparib, and standard paclitaxel and 20 percent for patients treated with control therapy.
Among the 73 patients, 21 had triple-negative breast cancer and the remainder had HR-positive, HER2-negative breast cancer. The improvement in the estimated pCR rate was greatest among those patients who had triple-negative breast cancer. The estimated pCR rates for patients with triple-negative breast cancer were 47 percent for those receiving durvalumab, olaparib, and standard paclitaxel and 27 percent for patients treated with control therapy. Among patients with HR-positive, HER2-negative breast cancer, the estimated pCR rates were 28 percent for those receiving durvalumab, olaparib, and standard paclitaxel and 14 percent for those in the control arm.
Based on the pCR data, Pusztai and colleagues calculated that there is an 81 percent probability that durvalumab and olaparib plus standard neoadjuvant chemotherapy would be statistically superior to standard neoadjuvant chemotherapy for patients with HER2-negative breast cancer in a 300-patient, randomized, phase III clinical trial. The probability of success would be 80 percent if such a trial enrolled only patients with triple-negative breast cancers and 74.5 percent if it enrolled only patients with HR-positive, HER2-negative breast cancers.
In her discussion of Pusztai’s presentation, Pamela Munster, MD, from the UCSF Helen Diller Family Comprehensive Cancer Center, noted that integrating immune checkpoint inhibitors into the treatment of early-stage breast cancer is an exciting area of research. She said that while the data shown suggest that adding durvalumab and olaparib to paclitaxel has promise, it remains to be determined how much of the benefit was conferred by olaparib. Munster concluded that it will require confirmatory randomized trials that include analysis of PD-L1 expression and BRCA mutation status before immune checkpoint inhibitor–PARP inhibitor combination therapies can be introduced as treatments for early-stage breast cancer.
The Challenge: Combining Immune Checkpoint Inhibitor and Antihormone Therapy for Prostate Cancer
Prostate cancer is the most commonly diagnosed cancer and the second most common cause of death among U.S. men, just as breast cancer is for women.
At the time of diagnosis, the growth of most prostate cancers is fueled by hormones called androgens, and treatments that either lower androgen levels in the body or stop androgens from affecting prostate cancer cells are initially successful for most men. Unfortunately, most prostate cancer cases eventually stop responding to treatment and progress, at which point the cancer is referred to as castration-resistant prostate cancer.
The second-generation antihormone agents abiraterone (Zytiga) and enzalutamide (Xtandi) are the mainstay of treatment for metastatic castration-resistant prostate cancer. New treatments are urgently needed, however, as just 30 percent of men who have metastatic prostate cancer are alive five or more years after diagnosis, according to the NCI.
One potential approach to improve outcomes for men with metastatic castration-resistant prostate cancer is to add an immune checkpoint inhibitor to treatment with a second-generation antihormone agent. Results from a randomized, phase III clinical trial in which this approach was tested were reported in the final presentation of the Opening Clinical Plenary by Christopher J. Sweeney, MBBS, from the Dana-Farber Cancer Institute in Boston.

In the trial, which was called IMbassador250, Sweeney and colleagues tested whether adding atezolizumab to enzalutamide improved survival for men with metastatic castration-resistant prostate cancer compared with enzalutamide alone. Unfortunately, it did not. The median overall survival among the 379 patients randomized to the combination treatment was 15.2 months and it was 16.6 months among those randomized to enzalutamide alone. As a result of these data, the clinical trial was terminated early.
Sweeney went on to say that an initial exploratory analysis of clinical subgroups revealed no evidence of overall survival benefit in any of the groups assessed, even the group with high levels of PDL1. However, “biomarker studies are ongoing,” according to a quote from a spokesperson for Genentech, which is a member of the Roche Group (Roche is the company that sponsored the trial), in a piece on FiercePharma about the IMbassador250 clinical trial.
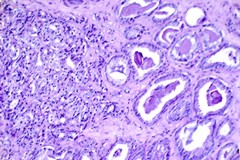
Padmanee Sharma, MD, PhD, from The University of Texas MD Anderson Cancer Center, who was the discussant of Sweeney’s presentation, talked about some of the lessons that can be learned from the results of the IMbassador250 clinical trial and the next steps for developing immune checkpoint inhibitor combination treatments for men who have metastatic castration-resistant prostate cancer. Sharma suggested that the tumor microenvironment might hold the answer as to why atezolizumab did not benefit patients with metastatic castration-resistant prostate cancer because:
- The tumor microenvironment in prostate cancer has very few T cells, therefore, releasing the brakes on T cells with atezolizumab might not be expected to result in the cancer being controlled.
- There are multiple immunosuppressive pathways in the prostate cancer tumor microenvironment, therefore, targeting a single pathway may not be enough to yield a tumor response.
- There are few mutations in prostate cancer, therefore, T cells may not recognize and target the cancer.
- The impact of enzalutamide on the immune response in the tumor microenvironment is unknown.
- The multiple previous treatments received by the patients may have impaired the ability of the patient’s immune cells to respond to atezolizumab.
- A combination of all of the above.
Sharma concluded by saying that she believes that “successful combination strategies will require in-depth studies to understand the impact of each agent and the combination on the tumor microenvironment before selecting the appropriate combination for phase III studies.”



