The Fungus Within Us: The Mycobiome’s Emerging Role in Cancer
What comes to mind when you think of a fungus? A mushroom? A case of athlete’s foot or ringworm?
How about cancer?
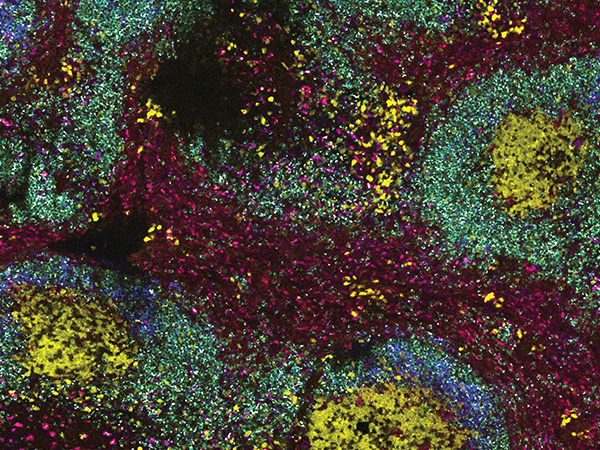
For years, researchers have explored the role of bacteria and viruses in cancer, demonstrating that these elements impact disease trajectories and treatment responses. Now, researchers have discovered that tumors and their surrounding milieu also house various fungal species—comprising what is known as the mycobiome—that could work in concert with bacteria, cellular proteins, and immune cells to influence cancer progression and patient prognosis.
According to two back-to-back cancer-wide analyses published in the September 2022 issue of Cell, fungi inhabit tumors arising in at least 35 different tissues, potentially relocating from the gut to other organs by way of the bloodstream. The compositions of cancer mycobiomes are tissue-specific, as are interactions formed between fungal communities and neighboring bacteria.

When the first evidence of fungi coexisting with cancer was reported in 2019 in pancreatic cancer, it was suggested that cancer-associated fungi might impact the onset and progression of this cancer type. At the AACR Annual Meeting 2022, and in an article published this year, researchers showed that in a subset of pancreatic cancers, fungi promoted the secretion of an immune-suppressing protein called IL-33, potentially enabling these cancers to circumvent the antitumor effects of the immune response and progress to more advanced stages. Interestingly, the expression of IL-33 was increased by a mutated form of the KRAS protein, thus revealing a tumor-promoting collaboration between this common mutant and the mycobiome in pancreatic cancer.
Building on these observations, the latest studies in Cell similarly identified correlations between fungi and cancer traits and outcomes. The presence of the Candida group of fungi, for example, was associated with inflammation and immune activation in stomach cancer, tumor-promoting gene expression changes in head-and-neck and colon cancers, metastasis in colon cancers, and reduced survival in various gastrointestinal cancers. Researchers found that interactions between fungi and surrounding bacterial communities correlated with outcomes, too.
Importantly, researchers could not determine whether the observed associations were causal. It is possible that the mycobiome directly or indirectly impacts tumor progression, but it is also feasible that fungal growth is a consequence of the environmental changes brought on by cancer development. Nonetheless, the recent findings could have important implications for cancer care.
A study from 2021 suggested that some fungi could negatively impact responses to radiation therapy by inhibiting antitumor immune functions, and studies from this year indicated that certain fungal species are associated with poor responses to immunotherapy in patients with melanoma. These findings raise the prospect of modulating the mycobiome to improve responses to cancer treatments.
Another idea is to utilize changes to the mycobiome as a biomarker of cancer onset or progression. Researchers showed that fungal DNA circulated in the blood, which might allow clinicians to screen for cancer by analyzing the mycobiome with just a simple blood draw.
While the relationship between the mycobiome and cancer is just beginning to be understood, it has become increasingly apparent that fungal species, like the bacteria and viruses studied before, could have a role in cancer, presenting new opportunities for treatment and disease monitoring.