December Highlights from AACR Journals
2023 is upon us, but before we dive into the new year, let’s look back at the featured articles from the December issues of the AACR’s 10 journals.
For the final 2022 installment of Editors’ Picks, the editors chose to highlight studies on how diabetes, physical activity, and obesity impact colorectal cancer risk; evaluation of investigational therapies and diagnostic biomarkers for pancreatic cancer; and insights into the effects of autophagy and the microbiome on cancer.
The studies are summarized below, and full details are found in the linked articles. As always, the articles will be freely available for a limited time.
Journal: Blood Cancer Discovery
Expansion of myeloblasts, which include CD34-positive hematopoietic stem and progenitor cells (HSPCs), is indicative of disease progression of chronic myeloid neoplasms, but it remains unclear what changes are associated with expansion and how these alterations impact clinical outcomes. Here, researchers aimed to characterize the changes that occur during myeloblast expansion. To this end, they examined transcription and immunophenotypes of CD34-positive HSPCs at the single-cell level at various stages of disease progression in 55 patients with chronic myelomonocytic leukemia. They found that HSPCs follow one of three differentiation trajectories: monocytic, megakaryocyte-erythroid progenitor, or normal-like. The monocytic-biased trajectory was associated with CD120-positive inflammatory granulocyte-macrophage progenitor cells, cytokine receptor signaling, depletion of stem cell markers, and adverse clinical outcomes. Hypomethylating agents suppressed the monocytic-biased trajectory in patients, while inflammation increased it in mouse models. The authors suggest that therapeutic strategies to suppress the monocytic differentiation trajectory should be explored. This article was highlighted in the December issue.
Journal: Cancer Discovery
In addition to directly killing tumor cells, radiation therapy can enhance antitumor immunity through the release of tumor-derived antigens. However, it is unclear whether this immune priming effect of radiation therapy is elicited in pancreatic cancer. Focal adhesion kinase (FAK) signaling is hyperactivated in pancreatic ductal adenocarcinoma (PDAC) and is implicated in the immunosuppressive and fibrotic microenvironment that causes poor drug delivery and dampens immune cell infiltration. Analyzing human PDAC tissues and mouse models, the authors of this study found that radiation therapy was not effective at priming robust T-cell responses, and that stromal components including fibroblasts and collagen were responsible for the reduced efficacy of radiation therapy and dampening the expression of interferon genes. Furthermore, FAK inhibition sensitized PDAC to radiation therapy in vitro and in vivo and enhanced the antitumor immune response, leading to tumor regression and increased survival in mouse models. Based on these observations, the authors initiated a clinical trial of the FAK inhibitor defactinib in combination with stereotactic body radiation therapy in patients with locally advanced PDAC. Analysis of tumor tissues from patients enrolled in the trial showed similar stromal changes observed in the mouse models. In addition, the combination of radiation therapy, FAK inhibition, and immune checkpoint blockade in mouse models led to tumor regression over time and long-term survival. This article was highlighted in the December issue.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Physical activity and obesity may increase colorectal cancer risk and impact patient prognosis, but the mechanisms behind these associations remain unclear. In this study, researchers examined how physical activity and/or body mass index (BMI) impacted various proinflammatory biomarkers in patients with colorectal cancer. The researchers utilized BMI data and self-reported physical activity levels from 579 patients enrolled in the ColoCare Study. Patients were classified as physically active if they had at least 8.75 hours of metabolic equivalent tasks per week and as physically inactive if they had less. Patients with obesity had significantly higher levels of C-reactive protein (CRP) and TNFα compared with those of healthy weight, and patients who were both overweight/obese and physically inactive had significantly higher CRP levels compared with those who had healthy weight and were physically active. IL-6 levels were also higher among patients who were physically inactive, but this difference was not statistically significant. Together, the results indicate that obesity, alone and in combination with physical inactivity, may lead to higher levels of proinflammatory biomarkers. This study was highlighted in the December issue.
Journal: Cancer Immunology Research
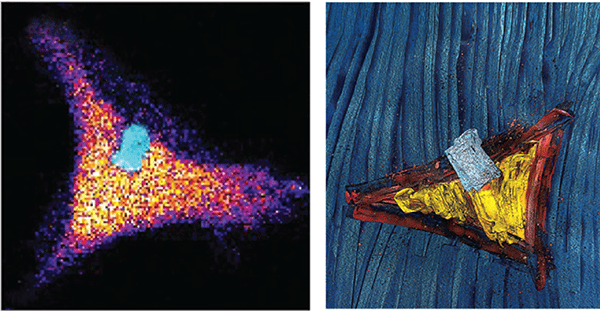
The success of immunotherapy strategies aimed at enhancing tumor infiltration by cytotoxic T lymphocytes (CTL) has been hampered by the existence of immunosuppressive factors in the tumor microenvironment, which interfere with CTL function. In this study, the authors focused on the nucleoside adenosine, and dissected the mechanisms through which it compromises CTL effector function. Applying time-resolved single-cell analyses in 3-D collagen co-cultures, the researchers found that adenosine destabilizes the contact between CTLs and tumor cells, resulting in reduced cell killing, and that selective inhibition of the adenosine A2a receptor (ADORA2a) signaling restored CTL killing function. ADORA2a antagonism also promoted CTL expansion and cytotoxicity toward melanoma tumors in in vivo models. According to the authors, these findings suggest that ADORA2a targeting may represent a strategy to reinvigorate CTLs and enhance immunotherapy efficacy. This article was featured on the cover of the December issue.
Journal: Cancer Prevention Research
Endoscopic Screening and Risk of Colorectal Cancer According to Type 2 Diabetes Status
The incidence rates of early-onset colorectal cancer and of early-onset type 2 diabetes have increased in recent decades. However, it is not known if type 2 diabetes impacts an individual’s risk of colorectal cancer or their potential benefit from cancer screening. Here, researchers used data from the Nurses’ Health Study I and II and the Health Professionals Follow-up Study to calculate endoscopic screening-associated absolute risk reductions for colorectal cancer incidence and mortality according to type 2 diabetes status. They found that endoscopic screening led to a greater reduction of colorectal cancer incidence and mortality among those who had type 2 diabetes compared with those who did not. Furthermore, individuals with type 2 diabetes had a similar risk of colorectal cancer at age 36 as those without type 2 diabetes at age 45. The authors propose that individuals with type 2 diabetes might benefit from earlier screening for colorectal cancer.
Journal: Cancer Research (December 1 issue)
Transient Systemic Autophagy Inhibition is Selectively and Irreversibly Deleterious to Lung Cancer
Autophagy within tumor cells and throughout the body promotes lung tumorigenesis by replenishing biomaterials and suppressing the antitumor immune response, respectively. Thus, there is interest in inhibiting autophagy to treat lung cancer, but previous studies have shown that sustained inhibition of autophagy can damage normal tissues. The authors of this study developed a novel mouse model that enabled them to induce deletion of the Atg gene to inhibit autophagy in a reversible manner in either tumor tissue or systemically. Using this model, they found that transient systemic, but not tumor-selective, inhibition of autophagy irreversibly suppressed the growth of KRAS-mutated and p53-deficient non-small cell lung cancer (NSCLC) cells, which represent 15-20 percent of all NSCLCs. The suppression of tumor growth occurred without affecting normal cells and was due to changes in metabolic processes, as well as to upregulation of the antitumor immune response. Together, the results suggest that temporary and systemic inhibition of autophagy could be an effective approach to treat this subset of lung cancers. A related commentary can be found here.
Journal: Cancer Research (December 15 issue)
Disruption of the Gut Microbiota Confers Cisplatin Resistance in Epithelial Ovarian Cancer
The composition of microbes in the digestive tract has far-reaching effects on the human body, and some studies have suggested that they may influence how a patient responds to cancer treatment. As many cancer patients receive antibiotics before or during cancer treatment, the authors of this study sought to assess whether antibiotics affect the response to cisplatin in mouse models of epithelial ovarian cancer. Mice began treatment with an antibiotic cocktail or a water control two weeks prior to ovarian cancer cell xenografting and cisplatin or a placebo two weeks after xenografting. In both cisplatin- and placebo-treated mice, survival was significantly longer in the control cohort than in the cohort that received antibiotics. Tumor samples harvested from antibiotic-treated mice revealed decreased expression of cisplatin-driven DNA damage markers and increased expression of stem cell-related genes compared with control-treated mice. These differences were observed in both immune competent and immunocompromised mice, and immune cell numbers were comparable in the ascites fluid and bone marrow of mice treated with or without antibiotics. A fecal transplant prior to cell xenografting from mice that did not receive antibiotics to those that did restored sensitivity to cisplatin. These results suggest that a patient’s microbiome may influence their response to cisplatin, and that a robust microbiome is necessary to confer cisplatin sensitivity in ovarian tumors. A commentary on this study is available here.
Journal: Clinical Cancer Research (December 1 issue)
In adults, the combination of the immune checkpoint inhibitors nivolumab (Opdivo) and ipilimumab (Yervoy) has led to greater responses than single-agent treatment, but this combination has not been evaluated in pediatric patients. In this article, the authors report results from a phase I/II clinical trial evaluating nivolumab plus ipilimumab in 55 children and young adults with recurrent or refractory solid tumors. Among the 41 patients who received treatment at the recommended phase II dose, two patients had sustained partial responses, and four patients had stable disease. Six patients experienced dose-limiting toxicities at the recommended phase II dose. Of the eight patients who received a higher dose of ipilimumab, three patients experienced dose-limiting toxicities, and no patients had an objective response. The authors conclude that the combination of nivolumab and ipilimumab at the recommended phase II dose is well tolerated and has signs of clinical activity in pediatric patients with solid tumors. This article was highlighted in the December 1 issue.
Journal: Clinical Cancer Research (December 15 issue)
Cervical cancer is commonly treated with a combination of chemotherapy and radiation, but hypoxia, which is common in cervical tumors, can decrease the efficacy of radiation. The diabetes drug metformin has been shown to decrease tumor hypoxia. In this phase II clinical trial, the researchers assessed whether metformin could decrease the hypoxic volume of cervical tumors. Thirteen patients with hypoxic tumors confirmed by PET imaging were randomly assigned to receive metformin plus chemoradiotherapy or chemoradiotherapy alone. One week after the start of treatment, the 10 patients receiving metformin experienced an average decrease in hypoxic volume of 10.2 percent, while the patients receiving chemoradiotherapy alone experienced an average increase in hypoxic volume of 4.7 percent. After an average follow-up of 3.3 years, the two-year median disease-free survival was 67 percent among metformin-treated patients and 33 percent among those treated with chemoradiotherapy alone. Although the differences between treatment arms were not significant due to the small sample size, the researchers suggested that further studies into metformin for hypoxic cervical cancer are warranted. This article was highlighted in the December 15 issue, and a related commentary is available.
Journal: Molecular Cancer Research
The genetic factors that increase susceptibility to hereditary prostate cancer remain unknown, particularly in African American families. In this study, researchers performed sequencing on two brothers, one with prostate cancer and one without, from an African American family with a history of prostate cancer. The novel variants identified through this analysis were further investigated in 20 additional African American families with a history of prostate cancer. Through these analyses, the researchers identified a germline mutation in the ADPRHL1 gene in four of the families; the mutation was found in many of the men affected by prostate cancer but not in 170 unrelated African American men without prostate cancer. Cell culture experiments determined that mutant ADPRHL1 activated PARP1 and increased DNA damage. Inhibition of PARP1 with olaparib suppressed proliferation of ADPRHL1-mutated prostate cancer cells, suggesting that mutant ADPRHL1 functions through PARP1 to foster prostate cancer survival. The authors propose that ADPRHL1 is a tumor suppressor and inherited loss-of-function mutation may increase susceptibility to prostate cancer in African American families. This article is highlighted in the December issue.
Journal: Molecular Cancer Therapeutics
BT8009; A Nectin-4 Targeting Bicycle Toxin Conjugate for Treatment of Solid Tumors
Antibody-drug conjugates (ADCs) are a popular form of targeted therapy but have limitations, such as large size, low tissue permeability, and off-target toxicity. Bicycle toxin conjugates (BTCs) use a small bicyclic peptide instead of an antibody to recognize their target of interest and can be cleaved by proteases in the microenvironment, eliminating the need for cell internalization. Ideally, these advantages increase the dose that can be safely delivered, boost tissue permeability, and enhance the bystander effect by which tumor cells that do not express the target can also be killed. In this study, the researchers characterized the BTC BT8009, consisting of a Nectin-4-targeting bicyclic peptide and the toxin mono-methylauristatin E (MMAE). In cell xenograft models, BT8009 accumulated in tumor tissue and remained at concentrations of around 100 pmol/g for 24-48 hours, despite being cleared rapidly from the plasma. A dose of 3 mg/kg, given weekly, induced tumor regression in both cell and patient-derived xenograft (PDX) mouse models of various tumor types, and the response positively correlated with Nectin-4 expression. The researchers also tested BT8009 alongside a Nectin-4 targeting ADC and showed that BT8009 elicited more rapid and/or robust tumor regression than the ADC in cell xenograft models of non-small cell lung cancer (NSCLC), triple negative breast cancer, and head and neck cancer, and a longer recurrence-free survival in a PDX model of NSCLC. Toxicities were mostly hematological, with no significant gastrointestinal, liver, or kidney adverse events observed. A phase I/II clinical trial of BT8009 in patients with advanced solid tumors is currently ongoing. This study was highlighted in and featured on the cover of the December issue.

Journal: Cancer Research Communications
Cancer Research Communications selected a double feature of Editors’ Picks for December, focusing on the diagnosis and treatment of pancreatic cancer. In one study, the researchers conducted a meta-analysis of 250 studies investigating blood-based biomarkers of pancreatic cancer. The researchers identified 982 individual biomarkers, including CA19-9, the only FDA-approved biomarker of pancreatic cancer. Around 60 percent of biomarkers had area under the curve (AUC) values listed and were included in the meta-analysis. The pooled AUC for biomarker panels was 0.898, significantly higher than the pooled AUC for individual biomarkers (0.803). Among biomarker panels containing CA19-9, the pooled AUC was 0.914, which was significantly higher than the pooled AUC for CA19-9 alone (0.85). The researchers identified a handful of biomarkers, including TIMP-1 and IL-8, which scored in the 90th percentile for both sensitivity and specificity; however, the researchers suggested that this study positions biomarker panels as superior to individual biomarkers, and that the markers comprising these panels must be carefully selected to optimize accuracy.
In the other study, the researchers explored new ways to treat pancreatic cancer by assessing the efficacy of the CDK4/6 inhibitor palbociclib (Ibrance) plus nab-paclitaxel (Abraxane) in preclinical models and in a phase Ib clinical trial. In three of four patient-derived xenograft mouse models, palbociclib plus nab-paclitaxel decreased tumor growth more effectively than gemcitabine (Gemzar) plus nab-paclitaxel, a standard-of-care treatment for patients who cannot tolerate FOLFIRINOX. In a clinical trial of 36 patients, the maximum tolerated dose (MTD) was defined as 100 mg per day for 21 of 28 days per treatment cycle plus weekly paclitaxel for three of the four weeks. Among patients who received the MTD as a first-line therapy, the overall response rate was 13 percent (all partial responses), the clinical benefit rate was 65.2 percent, and the median overall survival was 12.1 months. The prespecified efficacy threshold was a 65 percent or greater 12-month survival rate, and the 12-month survival rate among patients treated at the MTD was 50 percent.