AACR-NCI-EORTC Molecular Targets and Cancer Therapeutics Keynotes Highlight Basic and Clinical Research
Cancers are driven by unique genetic alterations, so what if we targeted these alterations to treat the cancer?
It seems straightforward, but it’s easier said than done.
The journey to treating cancer this way requires a fundamental understanding of what the cancer-driving mutations are and how they function, followed by the development of drugs that successfully block their activity. On the other end of the scientific continuum, robust clinical data are needed to understand how safe and effective these drugs are in patients and to identify the patients who may benefit the most.
The AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics, held October 11-15 in Boston, captured the full spectrum of research that goes into developing molecularly targeted cancer therapeutics, from the basic science that identifies targets to the clinical research that evaluates new drugs in patients.
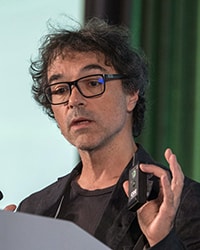
The breadth of the scientific program was exemplified by the meeting’s opening keynote lectures. Nobel Laureate William G. Kaelin Jr., MD, FAACR, of Dana-Farber Cancer Institute and Harvard Medical School, delivered a presentation on basic and translational research approaches to identify and drug new therapeutic targets, while Fabrice André, MD, PhD, of Gustave Roussy in France, discussed strategies for improving the treatment of patients.
Identifying new targets and therapeutic approaches
Kaelin began his presentation by noting that even in 2023, there are many who believe that targeting molecular alterations in cancer is a futile approach. They posit that there are too many driver mutations in any one cancer for targeted therapy to be successful, but Kaelin argued that it is possible to find a target that when blocked, is sufficient to kill cancer. He cited imatinib (Gleevec) as an example where this approach was successful.

Kaelin also noted that some mutations that develop at a later stage of cancer would be expected to kill the cancer cell but may be tolerated by the cell because of mutations that came earlier in the cancer’s evolution or earlier in a signaling pathway. Therefore, targeting an earlier mutation may be enough to kill the cancer, despite the existence of additional alterations.
As a paradigm of this hypothesis, Kaelin described his research on targeting HIF2α, a protein that regulates the cellular response to hypoxia. (Kaelin was a corecipient of the 2019 Nobel Prize in Physiology or Medicine for uncovering a link between HIF expression and cancer.)
In cancers harboring mutations in the VHL gene, HIF2α is overexpressed, leading to the downstream activation of VEGF and the formation of new blood vessels to foster cancer growth. Following the success of VEGF inhibitors, Kaelin and colleagues moved upstream and targeted HIF2α instead. They found that HIF2α inhibition was sufficient to suppress the growth of certain VHL-mutated kidney cancers.
The HIF2α inhibitor belzutifan (Welireg) is now approved for various VHL-driven malignancies. Ongoing clinical trials aim to identify biomarkers that predict response to belzutifan and evaluate belzutifan in combination with CDK4/6 inhibitors, Kaelin noted.
Kaelin also expanded on strategies for targeting the so-called “undruggable” proteins: targeting critical downstream effectors, using allosteric inhibitors, exploiting synthetic lethality, and using protein degrading molecules.
A popular tactic for finding synthetically lethal targets is to employ a CRISPR-based screen. However, one challenge is that paralog genes oftentimes compensate for the deleted gene, resulting in false negatives in the screen, Kaelin explained.
To circumvent this issue, he suggested simultaneously inactivating multiple paralogs, performing screens in simpler organisms that have fewer paralogs, and/or using chemical inhibitors of the proteins instead of genetic deletions. In addition, he raised the idea of achieving synthetic lethality in cancers driven by copy number loss by inhibiting the remaining gene copy just enough to render it inactive.
Kaelin also highlighted the potential of protein degraders—such as PROTACs, molecular glues, and degrons—for cancer treatment. In addition, he discussed screening mixtures of natural products as potential therapeutics and noted that removing contaminants from these mixtures will be critical for the success of such screens.
Finally, Kaelin discussed strategies for combination therapies. He noted that most successful combination therapies work through “bet hedging,” whereby increasing the number of therapeutics administered to a patient increases the likelihood that their cancer will respond to one of them. This concept, known as independent drug action, was discussed in a previous blog post.
Based on this, Kaelin proposed that combining drugs with distinct, nonoverlapping mechanisms of action may be a more effective approach than trying to find synergistic combinations.
“It may be inelegant, but … combining drugs with distinct mechanisms of action is the proven way to enhance efficacy while minimizing toxicity and minimizing therapeutic resistance,” he said.
Despite the doubts that some may have about targeted therapy, it’s clear that many patients are benefiting from this approach. To conclude, Kaelin shared remarks from patients who were successfully treated with a molecularly targeted therapy.
One patient, from a trip to Taiwan, declared, “If it wasn’t for the [belzutifan] drug trial, I would never have been able to come out here and do what I’m doing now.”
From another patient whose tumors disappeared after treatment: “I never thought I’d see this day.”
Improving the employment of molecularly targeted therapies
While cancers and their treatments have historically been categorized by organ site, André hopes the field will continue to move toward classifying cancers by their unique alterations and driver mechanisms.
“It’s time to move [toward] organ-agnostic, biomarker-based development of new drugs designed to hit a molecular target shared across cancers,” he said.
His keynote lecture summarized initiatives he and colleagues have undertaken in France to improve the employment of molecularly targeted therapies.
One initiative is to identify patients who have a high risk of cancer-related death. André explained that using artificial intelligence and tracking kinetics of circulating tumor DNA are two viable approaches to achieving this goal.
He highlighted one example that showed the potential of artificial intelligence to identify patients at high risk of death using tissue histology slides.
The second initiative is to identify an optimal therapeutic target for each patient’s tumor, which André believes will improve outcomes. To model the biology of a patient’s tumor, André proposed several different approaches, including multigene sequencing, ATAC-seq or CHIP-seq to study epigenetic reprogramming, spatial biology analyses to predict sensitivity of a therapy, examination of circulating tumor cells to monitor the cancer’s adaptation to therapy, and organoid models.
A recent trial showed that organoids could be successfully used to guide treatment for a patient with pancreatic cancer, André noted.
To accelerate the development of therapies for tumors with extremely rare mutations, André implored attendees to contribute clinical data of such tumors and relevant clinical trials to large genomic repositories, such as the AACR Project GENIE registry.
The third initiative André and colleagues are undertaking is to understand each drug’s mechanism of action and mechanism of resistance. The UNLOCK program is focused on studying the biological factors that impact a drug’s effectiveness. As part of the UNLOCK program, the DAISY trial examined trastuzumab deruxtecan (T-DXd), an antibody-drug conjugate that is used to treat HER2-overexpressing breast cancers.
Researchers analyzed T-DXd distribution and uptake in tumors with high, low, or no HER2 expression and found that the level of HER2 expression in the cancer affected the distribution and uptake of T-DXd, which correlated with the likelihood of treatment response and the extent of tumor shrinkage. Findings such as these could provide insight into drug efficacy and resistance in certain tumors and could guide treatment selection.
Conference Cochairs Emphasize Diversity of Scientific Program
As they welcomed attendees to the meeting’s opening session, the three cochairs of the conference—Timothy Yap, MBBS, PhD; E.G. Elisabeth de Vries, MD, PhD; and Tim Greten, MD—remarked on the breadth of research included in this year’s scientific program.
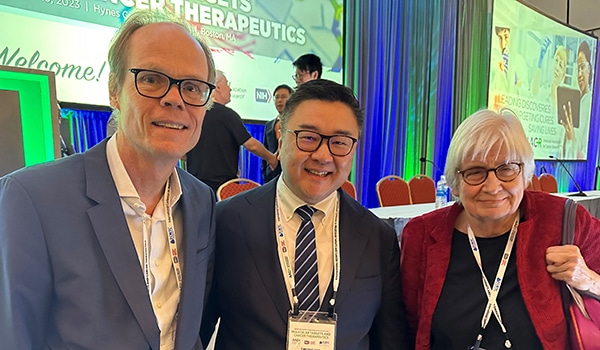
They noted that the presentations cover areas spanning from the early discovery of novel molecular targets all the way to clinical trials, as well as the inclusion of research from academic groups, biopharma/biotech companies, and historically underrepresented researchers.
“Finally, but maybe most importantly, we have graduate students, as well as Nobel Prize winners present in this room,” said Greten. “I very much look forward to the next four days.”
Stay tuned to the blog for more coverage from the AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics.