What Is Synthetic Lethality?
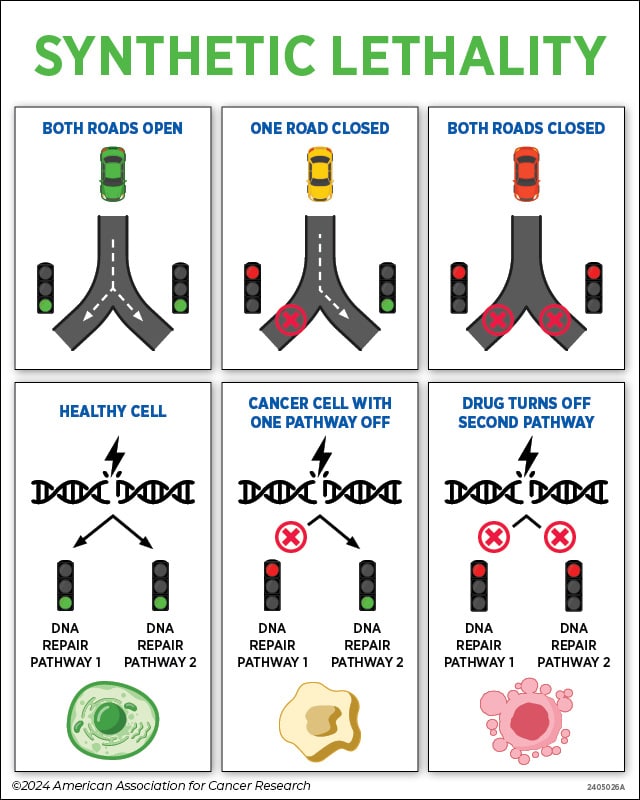
Imagine you’re driving home, and you come to a road closure on your normal route. Fortunately, another road that heads home is open, so you change routes and make it home easily.
But what if both roads were closed, and there was no way home?
This is the idea behind synthetic lethality, one of the many innovative strategies researchers are using to treat cancer.
Normally, cells fix routine damage to their DNA through different repair pathways. Some cancer cells, however, carry a mutation in a gene called BRCA that inactivates one of those repair pathways—essentially closing that “road.” Cancer cells with this mutation can still repair DNA damage through another repair pathway—a detour of sorts—allowing them to stay alive and keep growing.
Several years ago, researchers discovered that if they used a drug to block the “detour” repair pathway, then the cancer cells couldn’t repair the damage to their DNA. This caused the already unhealthy cells to become progressively unhealthier, which ultimately led to their death.
By “closing” both “roads,” the drug ended the cancer cells’ journey.
Which Treatments Use Synthetic Lethality?
Olaparib (Lynparza), the first drug to use this approach to treat cancer, was approved in 2014 to treat ovarian cancers that had a BRCA mutation. Olaparib works by inhibiting a DNA repair protein called PARP to shut off the “detour” repair pathway. Since the 2014 approval, olaparib and other PARP inhibitors have been approved to treat various BRCA-mutated cancers, either alone or in combination with other therapies.
- Olaparib is approved for certain ovarian, breast, pancreatic, and prostate cancers.
- Rucaparib (Rubraca) is approved for certain ovarian and prostate cancers.
- Niraparib (Zejula) is approved for certain ovarian, fallopian tube, or peritoneal cancers.
- Talazoparib (Talzenna) is approved for certain breast and prostate cancers.
Researchers continue to explore new synthetic lethality approaches to treat cancer—testing PARP inhibitors in different cancers, looking for additional drug targets in DNA repair pathways, and studying other cellular pathways that could drive synthetic lethality in cancers that carry other types of mutations.



