Colorectal Cancer Screening in the United States
A recent study revealed large variations in colorectal cancer screening rates among states and counties.
Colorectal cancer is the fourth most commonly diagnosed cancer in the United States with more than 135,000 diagnoses and over 50,000 deaths in 2017, according to federal statistics.
Despite those daunting numbers, the number of colorectal cancer cases has declined in recent years; it is thought that this decrease is due in part to an increase in awareness and screening.
March is Colorectal Cancer Awareness Month, a good time to raise awareness about the disease and guidelines for screening. The U.S. Preventive Services Task Force (USPSTF) recommends that most adults start getting screened for colorectal cancer at age 50, and continue this screening at regular intervals until age 75. Certain individuals may need to start screening earlier based on risk factors, including a family history of the disease.
While colonoscopy is the most well-known method to screen for colorectal cancer, other screening tests, such as flexible sigmoidoscopy and stool tests, can also detect the presence of cancer. Despite multiple screening methods, not everyone is up to date on their screening.
A study recently published in Cancer Epidemiology, Biomarkers & Prevention, a journal of the American Association for Cancer Research, estimated that over 30 percent of target adults (ages 50 to 75) were not current with colorectal cancer screening nationwide in 2014. The study also identified the states and counties that have low rates of screening in the U.S.
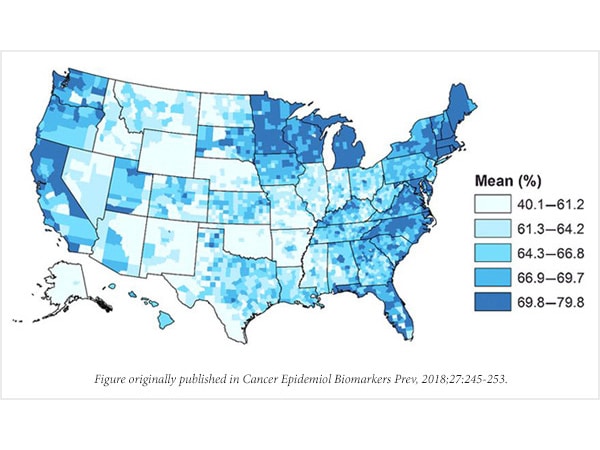
Researchers at the Centers for Disease Control and Prevention (CDC) generated models to estimate CRC screening rates in different states and counties. According to their state model, they estimated that Wyoming had the lowest rates of CRC screening while Massachusetts had the highest, at 58.9 percent and 75.0 percent, respectively.
Using their models, the researchers were also able to estimate colorectal cancer screening rates in all 3,142 U.S. counties. Variability between counties was high in some states, especially South Dakota, which had the highest variability at 28.6 percent.
“On a state level, our results identify counties where colorectal cancer screening rates are the lowest,” said lead author Zahava Berkowitz, MSPH, MSc, a statistician with the National Center for Chronic Disease Prevention and Health Promotion at the CDC. “These findings can help guide interventions that could increase colorectal cancer screening rates in these areas.”
Nationwide, there were also variabilities in colorectal cancer screening based on ethnicity. Non-Hispanic whites had higher screening rates than Hispanics (69.2 percent and 56.8 percent were current with screening, respectively).
This study highlights which populations – both geographically and racially – could most benefit from targeted interventions to increase colorectal cancer screening.
