From Autoimmune Disease to Cancer: Therapeutic Potential of Targeting PTPN22
The role of protein tyrosine phosphatase non-receptor type 22 (PTPN22) in T-cell receptor (TCR) signaling has thus far been primarily elucidated in the context of autoimmune diseases such as diabetes and rheumatoid arthritis (1). Won Jin Ho, MD, and his research colleagues demonstrated that genetic and pharmacological inhibition of PTPN22 retards tumor growth in a T-cell-and macrophage-dependent manner (2). Anti-tumor efficacy was also shown to be further increased by combining the novel PTPN22 inhibitor, L-1, with an anti-PD-1 antibody.
Dr. Won Jin Ho is currently an Assistant Professor at Johns Hopkins University. He received an AACR-Incyte Immuno-oncology Fellowship in 2019 as a second year medical oncology fellow. With the support of the AACR-Incyte fellowship and mentorship by Elizabeth M. Jaffee, MD, FAACR, he sought to elucidate the role of PTPN22 in antitumor immunity and to explore PTPN22’s therapeutic potential.
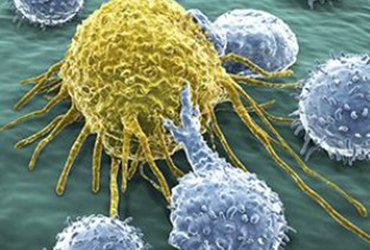
In his recent paper in the Journal of Clinical Investigation, Dr. Ho and his colleagues reported that tumor growth was stunted and immune cell infiltration into tumors was elevated in the absence of PTPN22. PTPN22 KO tumors had a higher percentage of T cells and tumor-associated macrophages (TAMs) in infiltrates than in WT tumors. Given the antitumor effects of PTPN22 knockdown, they screened a small collection of drug-like molecules for PTPN22 inhibitory activity and identified compound L-1. They then treated mice with L-1 and observed similar inhibition of tumor growth and increased immune cell infiltration. Through CD8+ T cell and TAM depletion experiments, they showed that the suppression of tumor growth in PTPN22 KO and L1-treated mice was dependent, at least in part, on CD8+ T cells and TAMs.
PTPN22 is known to inhibit TCR signaling by dephosphorylating Lck tyrosine kinase (Y934), Zap70 (Y493), and other players in the TCR signaling pathway (3). Phospho-profiling of tumor-infiltrating leukocytes showed that PTPN22 knockdown led to increased Lck phosphorylation (and activation) primarily of T cells of the early activated and central memory subtypes (i.e. early in CD8+ T cell differentiation). Higher phosphorylation levels at PTPN22-specific sites were associated with higher expression of the pro-immune cytokines IL-2 and IFNγ, the cytolytic molecule granzyme B, the activation marker CD69, and the checkpoint marker PD1.
In addition to enhancing tumor infiltration of TAMs, the lack of PTPN22 reprogrammed TAMs to be more antitumor M1-like which was dependent on CD8+ T cells. Co-culture experiments showed that the number of CD8+ cells was less suppressed when cultured with tumor-derived PTPN22 KO TAMs compared to WT TAMs. Instead, the PTPN22 KO TAMs enhanced T cell function and activation, as indicated by increased T-cell expression of IFNg.
PTPN22 KO induced an increase in PD-1 and Tbet expression by T cells and PD-1 expression by TAMs, portending a susceptibility to PD-1/PD-L1 pathway blockade. In vivo studies showed that the combination of either genetic or pharmacologic inhibition of PTPN22 with anti-PD-1 antibody had greater antitumor efficacy than either single agent alone. These laboratory experiments point to the possibility that a patient’s PTPN22 genotype/expression can be predictive of response to immune checkpoint blockade. The PTPN22 rs2476601 genetic variant has been associated with increased risk for multiple autoimmune diseases (4). Ho and his colleagues observed that patients with this genetic variant had significantly longer progression-free survival in response to anti-PD1 therapies than patients that did not have the variant.
These findings underscore the role of PTPN22 in anticancer immunity. The identification of a therapeutically promising PTPN22 inhibitor is welcome, given that protein tyrosine phosphatases have been considered undruggable for decades. As a drug that directly binds to the active site of PTPN22, L-1 may not only have an impact on treatment of cancer but also of autoimmune diseases.
References:
- Brownlie RJ, Zamoyska R, Salmon RJ. Immunology 2018; 154:377-382
- Ho WJ, Croessmann S, Lin J, Phyo ZW, Charmsaz S, Danilova L, et al. J Clin Invest 2021; 131: e146950
- Yang S, Svensson MND, Harder NHO, Hsieh W-C, Santelli E, Kiosses WB, et al. Science Signaling 2020; 13:eaaw8130
- Carlton VEH, Hu X, Chokkalingam AP, Schrodi SJ, Brandon R, Alexander HC, et al. Am J Hum Genet 2005; 77:567-81