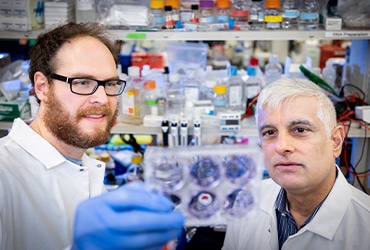
Sunil Hingorani and the Small Patients
When Sunil R. Hingorani, MD, PhD, was a young medical oncologist in training, educated at Yale and fresh off his clinical year at Dana-Farber, he cared for a patient with metastatic pancreatic cancer. He was well aware of the dismal outlook for people with pancreas cancer but hoped that his superb education and training could help the patient beat the odds.

The patient did better than most, but he succumbed to the disease in less than a year. Hingorani took it hard. After all, the patient was his own father – Ram Hingorani, a native of India.
“He was a gentleman who came to this country precisely so that his children could have opportunities that he did not have,” Hingorani recalls. “He and my mother provided all of those opportunities and then some, and the first and only time that he ever asked anything of me in his life, I failed him.”
Having worked in a laboratory that focused on the cancer-causing KRAS gene, Hingorani thought he knew something about pancreas cancer. Yet, his experience as his father’s doctor taught him that new approaches were needed, even if they were risky. Specifically, he concluded the traditional approach of running experiments in immortal cell lines wasn’t successful and had to go.
“I failed, but that also meant the system failed, my training failed, the experimental models we had at the time failed. When I made the decision that I was going to study pancreas cancer and only pancreas cancer, I knew for a fact that if I was going to fail, I wanted to fail spectacularly. I wanted to fail swinging for the fences, and I certainly did not want to fail 20 years, 30 years down the road with the exact same platforms that had already demonstrated their futility for several decades. We had to try another approach.”
As a postdoc with Tyler Jacks, PhD, at MIT and a junior faculty member at Penn, working with David Tuveson, MD, PhD, Hingorani helped develop the KPC mouse that faithfully recapitulates how pancreatic cancer develops.
When he had the opportunity to move to Fred Hutchinson Cancer Research Center in Seattle, he took it with the stipulation that he would see only pancreas cancer patients in the clinic and study only pancreas cancer in his lab.
To help get his lab going, he applied for and received the 2005 AACR-Pancreatic Cancer Action Network (PanCAN) career development award.
“The grant was focused on a very fundamental question around precursor lesions and the cell of origin of pancreas cancer, and it’s led to work that I’ve continued to pursue robustly since then,” he says. The grant work also set him up for several R01 and U01 grants, among others, that have sustained his lab over the years.
“That grant really launched a multi prong investigation into all aspects of this disease,” he says, and influences his work to the present day.
A major hurdle in pancreas cancer research is the sad fact that the disease is usually far advanced by the time the patient sees their doctor about a pain in the abdomen. Twenty years after Ram Hingorani lived longer than most patients, the median survival time from diagnosis is still less than a year, although some, of course, live much longer than that. But the typical patient might have one chance, at best, of participating in a clinical trial before the disease runs its course.
That’s where the mice come in – murine models, they are called, beady-eyed little stand-ins for human patients, genetically engineered to incorporate the events that occur in human patients.
“Creating a small patient that develops a disease that looks essentially identical to the disease in the large patient, and showing that something can work there, I think, has to be an important part of the process. For us, it’s the central part of the process,” he says, adding that people in his lab have a saying “Mice are people, too.”
In what they call a mouse hospital, Hingorani and his team conduct the Murine Clinical Trials Program (MCTP). Mice are used to carry out randomized, blinded, placebo-controlled trials that replicate human trials as much as possible. These include pilot studies, lasting from 14 to 28 days, intended to test treatment strategies. The strategies that show no signs of progress are abandoned, but the most promising ones can move on to the next level.
In full-blown survival studies, therapeutic agents are given to the mice at dosages equivalent to what humans get and administered the same way. Mice are palpated and imaged to identify primary tumor and metastases so they can be assigned to different arms of the study based on their disease burden, as humans would be assigned.
“We repeat an imaging study to measure objective response,” he says. “We follow the animals daily for symptoms, we weigh them, we look for signs of cachexia and how well they’re tolerating the regimen.”
(story continues below)
Since then, the field has grown; the funding picture has improved; meetings are held regularly, such as the AACR’s annual Special Conference on Pancreatic Cancer; and gains have been made in treatment. Combinations of drugs such as gemcitabine and nab-paclitaxel have helped bring incremental improvements, with five-year survival inching up to maybe 10 percent of patients. That gives him guarded optimism.
“We do mouse rounds in the MCTP. By the time a postdoc in the laboratory has rounded, say, for four to six months on mouse rounds, I can take them into the hospital, and they can round on patients with me and recognize all the same signs and symptoms in the patient that they learned from the pancreatic cancers that arise in these mice.”
Hingorani says that when he first contemplated specializing in pancreatic cancer, some of his mentors tried to dissuade him because funding was so scarce and progress in the disease was so lacking.
“This was an Incredibly lonely field,” he recalls.
“I do feel that we’re on the verge, with the understanding we’re developing, of creating combinatorial strategies that are going to have stepwise improvements in more dramatic chunks and increase survival in patients and truly change the way the disease is viewed,” he says.
“That’s my belief; that’s my hope; that sustains me. I don’t think it’s a vain hope. I think it’s a realistic one.”