AACR Journal Editors Share Selected Articles
As February gives way to March, we bring you the latest round of editors’ picks selected by the editors of AACR’s 10 journals. This month’s edition includes a new KRAS-targeting therapy for pancreatic cancer, an analysis of disparities in side effects between Black and white women receiving breast cancer treatment, final follow-up results from a phase III clinical trial, and more.
The abstracts of these selections are included below. As always, the full text of each article will be freely available for a limited time.
Journal: Blood Cancer Discovery
Genomic profiling revealed the identity of at least 5 subtypes of diffuse large B-cell lymphoma (DLBCL), including the MCD/C5 cluster characterized by aberrations in MYD88, BCL2, PRDM1, and/or SPIB. We generated mouse models harboring B cell–specific Prdm1 or Spib aberrations on the background of oncogenic Myd88 and Bcl2 lesions. We deployed whole-exome sequencing, transcriptome, flow-cytometry, and mass cytometry analyses to demonstrate that Prdm1- or Spib-altered lymphomas display molecular features consistent with prememory B cells and light-zone B cells, whereas lymphomas lacking these alterations were enriched for late light-zone and plasmablast-associated gene sets. Consistent with the phenotypic evidence for increased B cell receptor signaling activity in Prdm1-altered lymphomas, we demonstrate that combined BTK/BCL2 inhibition displays therapeutic activity in mice and in five of six relapsed/refractory DLBCL patients. Moreover, Prdm1-altered lymphomas were immunogenic upon transplantation into immuno-competent hosts, displayed an actionable PD-L1 surface expression, and were sensitive to antimurine-CD19-CAR-T cell therapy, in vivo.
A commentary related to this study can be found here.
Journal: Cancer Discovery
Efficacy of a Small-Molecule Inhibitor of KrasG12D in Immunocompetent Models of Pancreatic Cancer
Mutations in the KRAS oncogene are found in more than 90% of patients with pancreatic ductal adenocarcinoma (PDAC), with Gly-to-Asp mutations (KRASG12D) being the most common. Here, we tested the efficacy of a small-molecule KRASG12D inhibitor, MRTX1133, in implantable and autochthonous PDAC models with an intact immune system. In vitro studies validated the specificity and potency of MRTX1133. In vivo, MRTX1133 prompted deep tumor regressions in all models tested, including complete or near-complete remissions after 14 days. Concomitant with tumor cell apoptosis and proliferative arrest, drug treatment led to marked shifts in the tumor microenvironment (TME), including changes in fibroblasts, matrix, and macrophages. T cells were necessary for MRTX1133’s full antitumor effect, and T-cell depletion accelerated tumor regrowth after therapy. These results validate the specificity, potency, and efficacy of MRTX1133 in immunocompetent KRASG12D-mutant PDAC models, providing a rationale for clinical testing and a platform for further investigation of combination therapies.
This study was featured on the cover of the February issue, and a related commentary is available here.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Background: Symptom burden differences may contribute to racial disparities in breast cancer survival. We compared symptom changes from before to during chemotherapy among women with breast cancer.
Methods: This observational study followed a cohort of Black and White women diagnosed with Stage I–III, hormone receptor–positive breast cancer from a large cancer center in 2007 to 2015, and reported symptoms before and during chemotherapy. We identified patients who experienced a one-standard deviation (SD) increase in symptom burden after starting chemotherapy using four validated composite scores (General Physical Symptoms, Treatment Side Effects, Acute Distress, and Despair). Kitagawa–Blinder–Oaxaca decomposition was used to quantify race differences in symptom changes explained by baseline characteristics (sociodemographic, baseline scores, cancer stage) and first-line chemotherapy regimens.
Results: Among 1,273 patients, Black women (n = 405, 31.8%) were more likely to report one-SD increase in General Physical Symptoms (55.6% vs. 48.2%, P = 0.015), Treatment Side Effects (74.0% vs. 63.4%, P < 0.001), and Acute Distress (27.4% vs. 20.0%, P = 0.010) than White women. Baseline characteristics and first-line chemotherapy regimens explained a large and significant proportion of the difference in Acute Distress changes (93.7%, P = 0.001), but not General Physical Symptoms (25.7%, P = 0.25) or Treatment Side Effects (16.4%, P = 0.28).
Conclusions: Black women with early-stage breast cancer were more likely to experience significant increases in physical and psychological symptom burden during chemotherapy. Most of the difference in physical symptom changes remained unexplained by baseline characteristics, which suggests inadequate symptom management among Black women.
Impact: Future studies should identify strategies to improve symptom management among Black women and reduce differences in symptom burden.
This article was highlighted in the February issue, and a related commentary is available here.
Journal: Cancer Immunology Research
Rational Protein Design Yields a CD20 CAR with Superior Antitumor Efficacy Compared with CD19 CAR
Chimeric antigen receptors (CAR) are fusion proteins whose functional domains are often connected in a plug-and-play manner to generate multiple CAR variants. However, CARs with highly similar sequences can exhibit dramatic differences in function. Thus, approaches to rationally optimize CAR proteins are critical to the development of effective CAR T-cell therapies. Here, we report that as few as two amino-acid changes in nonsignaling domains of a CAR were able to significantly enhance in vivo antitumor efficacy. We demonstrate juxtamembrane alanine insertion and single-chain variable fragment sequence hybridization as two strategies that could be combined to maximize CAR functionality, and describe a CD20 CAR that outperformed the CD19 CAR in antitumor efficacy in preclinical in vitro and in vivo assays. Precise changes in the CAR sequence drove dramatically different transcriptomic profiles upon antigen stimulation, with the most efficacious CAR inducing an enrichment in highly functional memory T cells upon antigen stimulation. These findings underscore the importance of sequence-level optimization to CAR T-cell function, and the protein-engineering strategy described here may be applied to the development of additional CARs against diverse antigens.
A commentary related to this study is available here.
Journal: Cancer Prevention Research
Obesity and metabolic dysfunction are implicated in colorectal cancer development. Appetite-regulating gut hormones might have a role in colorectal cancer risk. We investigated whether circulating levels of the gut hormones ghrelin (analyzed as acyl ghrelin) and Peptide YY (PYY) were associated with subsequent colorectal cancer risk, including clinical and molecular tumor subtypes. We also provide descriptive data on these hormones in relation to background participant characteristics and metabolic biomarkers. This population-based study included 1,010 matched case–control pairs with a median of 12.3 years of follow-up. Acyl ghrelin and PYY were measured by multiplex immunoassay. Data on KRAS and BRAF mutations and microsatellite instability (MSI) status were available for 704 and 708 cases, respectively. Conditional logistic regression models estimated association to colorectal cancer risk. Partial correlation and linear regression were used to investigate relationships between background and metabolic variables and variation in plasma gut hormone concentrations. Acyl ghrelin was not clearly associated with colorectal cancer risk (multivariable OR per 1 SD increase: 1.11; 95% CI, 1.00–1.23). Positive associations were observed for specific subtypes, in particular BRAF-mutated colorectal cancer and right-sided colon cancer, although with nonsignificant heterogeneity. PYY was not related to colorectal cancer risk (multivariable OR per 1 SD: 1.04; 95% CI, 0.95–1.14) or any tumor subtype. In the control participants, ghrelin was inversely correlated with BMI, and PYY was positively correlated with C-peptide and insulin levels. These findings provide limited support for a possible role for ghrelin in colorectal cancer development, primarily in specific anatomical and molecular tumor subtypes.
Journal: Cancer Research (February 1 issue)
RNA editing modifies single nucleotides of RNAs, regulating primary protein structure and protein abundance. In recent years, the diversity of proteins and complexity of gene regulation associated with RNA editing dysregulation has been increasingly appreciated in oncology. Large-scale shifts in editing have been observed in bulk tumors across various cancer types. However, RNA editing in single cells and individual cell types within tumors has not been explored. By profiling editing in single cells from lung adenocarcinoma biopsies, we found that the increased editing trend of bulk lung tumors was unique to cancer cells. Elevated editing levels were observed in cancer cells resistant to targeted therapy, and editing sites associated with drug response were enriched. Consistent with the regulation of antiviral pathways by RNA editing, higher editing levels in cancer cells were associated with reduced antitumor innate immune response, especially levels of natural killer cell infiltration. In addition, the level of RNA editing in cancer cells was positively associated with somatic point mutation burden. This observation motivated the definition of a new metric, RNA editing load, reflecting the amount of RNA mutations created by RNA editing. Importantly, in lung cancer, RNA editing load was a stronger predictor of patient survival than DNA mutations. This study provides the first single cell dissection of editing in cancer and highlights the significance of RNA editing load in cancer prognosis.
A commentary related to this study is available here.
Journal: Cancer Research (February 15 issue)
Mutagenic processes leave distinct signatures in cancer genomes. The mutational signatures attributed to APOBEC3 cytidine deaminases are pervasive in human cancers. However, data linking individual APOBEC3 proteins to cancer mutagenesis in vivo are limited. Here, we showed that transgenic expression of human APOBEC3G promotes mutagenesis, genomic instability, and kataegis, leading to shorter survival in a murine bladder cancer model. Acting as mutagenic fuel, APOBEC3G increased the clonal diversity of bladder cancer, driving divergent cancer evolution. Characterization of the single base substitution signature induced by APOBEC3G in vivo established the induction of a mutational signature distinct from those caused by APOBEC3A and APOBEC3B. Analysis of thousands of human cancers revealed the contribution of APOBEC3G to the mutational profiles of multiple cancer types, including bladder cancer. Overall, this study dissects the mutagenic impact of APOBEC3G on the bladder cancer genome, identifying it contributes to genomic instability, tumor mutational burden, copy-number loss events, and clonal diversity.
This study was featured on the cover of the February 15 issue, and a related commentary is available here.
Journal: Clinical Cancer Research (February 1 issue)
Purpose: This study aimed to identify baseline clinical features associated with the outcomes of patients enrolled in the COMBI-MB phase II study of dabrafenib and trametinib treatment in patients with V600 BRAF-mutant metastatic melanoma with melanoma brain metastases (MBM). Exploratory biomarker analysis was also conducted as part of the synergistic COMBI-BRV trial (BRV116521), to identify molecular and immunologic changes associated with dabrafenib in MBMs and extracranial metastases (ECM).
Patients and Methods: Post hoc analysis was performed for baseline features of patients (n = 125) enrolled in COMBI-MB. Analyses were performed to identify baseline clinical features associated with intracranial response rate (ICRR), progression-free survival (PFS), and overall survival (OS). Exploratory biomarker analysis was performed on biospecimen collected in the COMBI-BRV trial in which patients with BRAF-mutant, resectable MBM were treated with dabrafenib for 10 to 14 days prior to craniotomy. Accessible ECM were resected or biopsied at the time of craniotomy. Biospecimens underwent molecular and immunologic profiling for comparative analyses.
Results: In COMBI-MB baseline treatment with corticosteroids was independently associated with lower ICRR [39% vs. 63%; OR, 0.323; 95 % confidence interval (CI), 0.105–0.996; P = 0.049] and shorter PFS (HR, 1.93; 95% CI, 1.06–3.51; P = 0.031). Additional significant associations identified in the multivariate analysis were improved PFS in patients with a BRAFV600E genotype (HR, 0.565; 95% CI, 0.321–0.996; P = 0.048) and improved OS in patients with Eastern Cooperative Oncology Group 0 (HR, 0.44; 95% CI, 0.25–0.78; P = 0.005).
Conclusions: Corticosteroid treatment was associated with reduced ICRR and PFS in COMBI-MB, similar to results with immunotherapy for MBMs. Baseline corticosteroid treatment is a key factor to consider in MBM patient management and clinical trial design/interpretation.
This article was highlighted in the February 1 issue.
Journal: Clinical Cancer Research (February 15 issue)
Five-Year Clinical Outcomes After Neoadjuvant Nivolumab in Resectable Non-Small Cell Lung Cancer
Purpose: Neoadjuvant anti–PD-1 therapy has shown promise for resectable non–small cell lung cancer (NSCLC). We reported the first phase I/II trial of neoadjuvant nivolumab in resectable NSCLC, finding it to be safe and feasible with encouraging major pathological responses (MPR). We now present 5-year clinical outcomes from this trial, representing to our knowledge, the longest follow-up data for neoadjuvant anti–PD-1 in any cancer type.
Patients and Methods: Two doses of nivolumab (3 mg/kg) were administered for 4 weeks before surgery to 21 patients with Stage I–IIIA NSCLC. 5-year recurrence-free survival (RFS), overall survival (OS), and associations with MPR and PD-L1, were evaluated.
Results: With a median follow-up of 63 months, 5-year RFS and OS rates were 60% and 80%, respectively. The presence of MPR and pre-treatment tumor PD-L1 positivity (TPS ≥1%) each trended toward favorable RFS; HR, 0.61 [95% confidence interval (CI), 0.15–2.44] and HR, 0.36 (95% CI, 0.07–1.85), respectively. At 5-year follow-up, 8 of 9 (89%) patients with MPR were alive and disease-free. There were no cancer-related deaths among patients with MPR. In contrast, 6/11 patients without MPR experienced tumor relapse, and 3 died.
Conclusions: Five-year clinical outcomes for neoadjuvant nivolumab in resectable NSCLC compare favorably with historical outcomes. MPR and PD-L1 positivity trended toward improved RFS, though definitive conclusions are limited by cohort size.
This study was highlighted in the February 15 issue and was the subject of a recent AACR press release.
Journal: Molecular Cancer Research
Small-cell lung cancer (SCLC) is a recalcitrant malignancy that urgently needs new therapies. Four master transcription factors (ASCL1, NEUROD1, POU2F3, and YAP1) have been identified in SCLC, and each defines the transcriptome landscape of one molecular subtype. However, these master transcription factors have not been found directly druggable. We hypothesized that blocking their transcriptional coactivator(s) could provide an alternative approach to target these master transcription factors. Here, we identify that BET proteins physically interact with NEUROD1 and function as transcriptional coactivators. Using CRISPR knockout and ChIP-seq, we demonstrate that NEUROD1 plays a critical role in defining the landscapes of BET proteins in the SCLC genome. Blocking BET proteins by inhibitors led to broad suppression of the NEUROD1-target genes, especially those associated with superenhancers, resulting in the inhibition of SCLC growth in vitro and in vivo. LSAMP, a membrane protein in the IgLON family, was identified as one of the NEUROD1-target genes mediating BET inhibitor sensitivity in SCLC. Altogether, our study reveals that BET proteins are essential in regulating NEUROD1 transactivation and are promising targets in SCLC-N subtype tumors.
This study was highlighted in the February issue.
Journal: Molecular Cancer Therapeutics
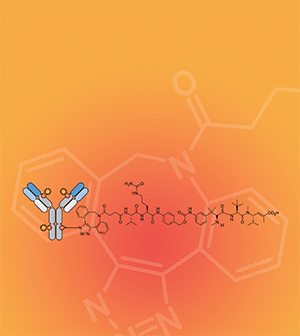
STRO-002 is a novel homogeneous folate receptor alpha (FolRα) targeting antibody–drug conjugate (ADC) currently being investigated in the clinic as a treatment for ovarian and endometrial cancers. Here, we describe the discovery, optimization, and antitumor properties of STRO-002. STRO-002 was generated by conjugation of a novel cleavable 3-aminophenyl hemiasterlin linker-warhead (SC239) to the nonnatural amino acid para-azidomethyl-L-phenylalanine incorporated at specific positions within a high affinity anti-FolRα antibody using Sutro’s XpressCF+, which resulted in a homogeneous ADC with a drug–antibody ratio (DAR) of 4. STRO-002 binds to FolRα with high affinity, internalizes rapidly into target positive cells, and releases the tubulin-targeting cytotoxin 3-aminophenyl hemiasterlin (SC209). SC209 has reduced potential for drug efflux via P-glycoprotein 1 drug pump compared with other tubulin-targeting payloads. While STRO-002 lacks nonspecific cytotoxicity toward FolRα-negative cell lines, bystander killing of target negative cells was observed when cocultured with target positive cells. STRO-002 is stable in circulation with no change in DAR for up to 21 days and has a half-life of 6.4 days in mice. A single dose of STRO-002 induced significant tumor growth inhibition in FolRα-expressing xenograft models and patient-derived xenograft models. In addition, combination treatment with carboplatin or Avastin further increased STRO-002 efficacy in xenograft models. The potent and specific preclinical efficacy of STRO-002 supports clinical development of STRO-002 for treating patients with FolRα-expressing cancers, including ovarian, endometrial, and non–small cell lung cancer. Phase I dose escalation for STRO-002 is in progress in ovarian cancer and endometrial cancer patients (NCT03748186 and NCT05200364).
This study was highlighted and featured on the cover of the February issue.
Journal: Cancer Research Communications
Markers of genomic instability, including TP53 status and homologous recombination deficiency (HRD), are candidate biomarkers of immunogenicity and immune-mediated survival, but little is known about the distribution of these markers in large, population-based cohorts of racially diverse patients with breast cancer. In prior clinical trials, DNA-based approaches have been emphasized, but recent data suggest that RNA-based assessment can capture pathway differences conveniently and may be streamlined with other RNA-based genomic risk scores. Thus, we used RNA expression to study genomic instability (HRD and TP53 pathways) in context of the breast cancer immune microenvironment in three datasets (total n = 4,892), including 1,942 samples from the Carolina Breast Cancer Study, a population-based study that oversampled Black (n = 1,026) and younger women (n = 1,032). Across all studies, 36.9% of estrogen receptor (ER)-positive and 92.6% of ER-negative breast cancer had presence of at least one genomic instability signature. TP53 and HRD status were significantly associated with immune expression in both ER-positive and ER-negative breast cancer. RNA-based genomic instability signatures were associated with higher PD-L1, CD8 T-cell marker, and global and multimarker immune cell expression. Among tumors with genomic instability signatures, adaptive immune response was associated with improved recurrence-free survival regardless of ER status, highlighting genomic instability as a candidate marker for predicting immunotherapy response. Leveraging a convenient, integrated RNA-based approach, this analysis shows that genomic instability interacts with immune response, an important target in breast cancer overall and in Black women who experience higher frequency of TP53 and HR deficiency.