AACR Annual Meeting 2023: The Past, Present, and Future of Targeted Therapies for Pediatric Cancer
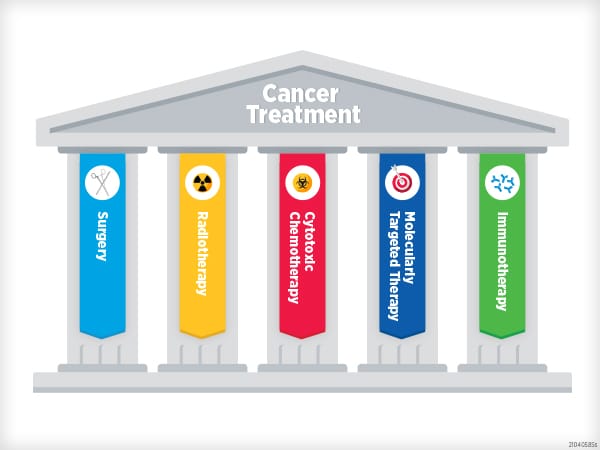
Historically, most cancer drugs have been tested separately in adults and children.
For the approval of new drugs for children, researchers must ensure that doses are properly recalculated and new side effects do not emerge in a younger population. However, for rare pediatric cancers with even rarer genetic mutations, it can be difficult to recruit enough participants to conduct a meaningful clinical trial.
In response to mounting evidence that therapies approved to target adult cancers with certain mutations are often effective in pediatric cancers with the same mutations, researchers and regulatory agencies are working to ensure more pediatric patients become eligible for lifesaving therapies. At the AACR Annual Meeting 2023, held in Orlando April 14-19, researchers showcased cutting-edge trials that are matching pediatric patients with therapies tailored to their tumors.
Here, we reflect on the changes in regulatory policy and clinical trial design that led to such studies, and we highlight the ways that creative thinking may broaden the scope of targeted therapies available for pediatric patients.
The Past: Before the Research to Accelerate Cures and Equity for Children Act
In 2020, the U.S. Food and Drug Administration (FDA) instituted the Research to Accelerate Cures and Equity (RACE) for Children Act, which requires more drug developers to test new drugs in pediatric patients. Prior to the passage of this act, if the drug target was primarily relevant in adult cancers, drug developers could apply for a waiver allowing them to exclude pediatric patients from their clinical trials. Now, as a result of the RACE Act, if any evidence exists that the molecular target of the drug is relevant in pediatric cancers, such waivers cannot be granted.
The rule includes new drugs with an orphan drug designation, meaning the company developing the drug is receiving a financial incentive from the federal government to aid in the treatment of rare diseases. Before RACE, orphan drugs were automatically exempt from pediatric testing.
Between the Congressional approval of the RACE Act and its implementation, a group of researchers studied the potential real-world impacts of the act. Of the 78 drugs approved by the FDA for adult cancer indications between 2007 and 2017, the researchers estimated that the RACE Act would have required 78.2% of them to be tested in children.
Another group of researchers evaluated how the first year of the RACE Act impacted studies of new drugs on pediatric patients. In the study, which was presented at the AACR Annual Meeting 2022, the researchers examined all new oncology drug applications or biologics license applications approved by the FDA in the year immediately prior to and the year immediately following implementation of the RACE Act.
In the year before RACE took effect, 8.3% of new drugs were indicated for use in pediatric patients; however, all of these drugs were either granted a waiver for pediatric testing or were exempt due to the orphan drug designation.
In contrast, 42.9% of new drugs approved after RACE were required to include pediatric patients in their studies. This included 60% of the drugs that received an orphan drug designation.
The U.S. Government Accountability Office has also evaluated the effects of the RACE Act on proposed and ongoing studies in pediatric patients. Their study found that, in the first two years of the act, 32 drug sponsors submitted pediatric study plans to the FDA; 25 of those drugs would have received an exemption or waiver for pediatric evaluation before the act.
The researchers interviewed several scientists, patient advocates, and drug developers who were optimistic about the potential effects of the RACE Act on pediatric cancer research and drug development. Several stakeholders mentioned seeing an increased interest in pediatric cancer research, including more inquiries about conducting pediatric cancer clinical trials.
The FDA responded with some ways they are working to help researchers optimize clinical testing in children. Ideas included learning from European colleagues who, having operated under legislation similar to the RACE Act for several years, are employing innovative clinical trial designs to expand treatment options for pediatric patients.
The Present: The MAPPYACTS Trial
Pediatric cancers are relatively rare, and those driven by mutations for which targeted therapeutics are available are even rarer. While most first-line therapies for pediatric cancers are based on chemotherapy and radiation, if tumors relapse, options for further treatment are limited. Identifying a targetable mutation in a child’s cancer could present new possibilities, but connecting children with appropriate clinical trials can present challenges.
An international European research group designed a clinical trial in which pediatric patients with a variety of relapsed or refractory tumor types could be genetically tested and matched with an appropriate targeted therapy. The MAPPYACTS trial, led by Birgit Geoerger, MD, PhD, a professor of pediatric clinical research at Gustave Roussy Cancer Center in France, enrolled over 600 pediatric cancer patients to evaluate their eligibility for targeted therapies.
“The main purpose was to genetically profile the patients’ tumors and use that to suggest a treatment,” Geoerger said in a press release about the study, which was published in Cancer Discovery, a journal of the AACR, in March 2022. “Are there molecular alterations that we can target with these newer drugs?”

MD, PhD
A clinical molecular tumor board reviewed the sequencing data from each patient and identified 432 patients with potentially actionable alterations—those with evidence that a drug could target the mutated protein or another member of the affected signaling pathway. Of these patients, 107 were treated with a matched targeted therapy, either alone or in combination with other therapies, as determined by the molecular tumor board.
Seventeen percent of treated patients experienced a complete or partial response, and 41% experienced stable disease. The overall response rate was higher—38%—among patients whose tumor mutations were considered “ready for routine use,” indicating that an approved drug had significant clinical evidence of its ability to treat cancers harboring the mutation.
Notably, 42% of “ready for routine use” alterations had not been identified by prior genomic or clinical testing. Geoerger emphasized that this highlights the need to critically evaluate relapsed or refractory pediatric cancers to identify all possible drug targets. “It didn’t mean an alteration couldn’t be found, rather that no one looked for it,” she said in the press release.
While these results support the prevailing belief that targeted therapies that are effective in adult tumors are often effective against the same mutations in pediatric tumors, the complex mutational landscape of pediatric tumors can sometimes convolute straightforward attempts to treat children’s cancers using targeted therapies. Geoerger and colleagues recognized that, in certain instances, more creative solutions may be necessary.
The Future: Creative Drug Targeting in AcSé-ESMART
Geoerger also leads a clinical trial called AcSé-ESMART, another international European proof-of-concept trial intended to match pediatric patients with a treatment regimen personalized to their mutational profile. AcSé-ESMART uses a patient’s sequencing data to assign them to one of several treatment arms designed to test new combination therapies in patients whose tumors may be driven by mutations in distinct cell signaling pathways.
In pediatric cancers, applying a targeted therapy approach can be more complicated than using a single drug to target a single mutation, said Susanne Gatz, MD, PhD, an associate clinical professor in pediatric oncology at the Institute of Cancer and Genomic Sciences of the University of Birmingham in the United Kingdom, who presented preliminary results from arm N of the AcSé-ESMART trial at the Annual Meeting 2023.
Gatz explained that while trials like MAPPYACTS have shown success in cases where pediatric tumors harbor the same genetic alterations as adult tumors, these cases comprise the minority of childhood cancers. More often, it is difficult to determine which mutations are driving a pediatric tumor, and in some instances, the mutated proteins cannot be targeted directly.

For example, arm N of AcSé-ESMART is tailored toward patients with malignancies that exhibit defects in homologous recombination, a type of DNA damage repair. In adults, such defects are often caused by mutations in BRCA1 or BRCA2, but these mutations are rare in pediatric tumors. Nevertheless, some pediatric tumors harbor other mutations in the homologous recombination pathway that may sensitize the tumors to drugs called PARP inhibitors.
While single-agent therapy with PARP inhibitors has had limited efficacy in pediatric patients, Gatz and colleagues hypothesized that another characteristic of pediatric cancer cells may help two drugs form an effective combination.
“Pediatric cancer cells proliferate rapidly and have some element of replication stress and a dependency on ATR,” Gatz said in a press release about the study. “We think there might be a kind of primary resistance of pediatric cancers to PARP inhibitors and that combination with an ATR inhibitor could potentially overcome that.”
To test their hypothesis, Gatz and colleagues enrolled 18 pediatric and young adult patients with relapsed or treatment-refractory solid tumors into the phase I portion of arm N. The tumors had undergone whole-exome sequencing and were found to have mutations that may confer homologous recombination deficiencies or DNA replication stress. Patients were treated with various dose levels of the PARP inhibitor olaparib (Lynparza) and the investigational ATR inhibitor ceralasertib to determine the recommended phase II dose.
One patient with pineoblastoma received 11 cycles of treatment and experienced a partial response. Another patient with neuroblastoma experienced stable disease until cycle 9, at which point their disease converted to a partial response. This patient continues to receive treatment in cycle 12, and three additional patients with stable disease—two in cycle 8 and one in cycle 15—also remain on treatment.
Gatz emphasized that, moving forward, the researchers will focus on identifying additional biomarkers of response to olaparib plus ceralasertib that may help them better understand the mechanisms of response and define who is most likely to respond. She and her colleagues intend to move beyond DNA sequencing and into a multiomics approach that includes data from immunohistochemistry and RNA sequencing.
“So far, it is unclear if the molecular alterations based on which the patients were enrolled in this trial are the sole reasons for response,” Gatz said in the press release. “Nevertheless, this study design can give preliminary indications of signals in specific alterations and tumor types and can provide the basis for future clinical trials.”
Content from the AACR Annual Meeting 2023 will be available on the virtual meeting platform to registered participants for three months after the meeting. Visit the registration page for more information.