Detecting Cancer with Body Fluids Other Than Blood
Ancient Greek physician Hippocrates considered the human body to be a system composed of four balanced fluids, or “humours.” The theory has long been supplanted, but contemporary oncology has brought body fluids back into vogue with their use as sources of information that can signal the presence of cancer.
The term liquid biopsy refers to the detection and analysis of tumor biomarkers present in the blood—such as circulating tumor DNA (ctDNA), circulating tumor cells, and exosomes. However, studies have shown that several other body fluids contain tumor-derived molecules and could represent additional sources for liquid biopsy applications.
For example, researchers have explored leveraging saliva to detect oral, pancreatic, lung, ovarian, and breast cancer. Due to its abundance and ease of collection, many studies have focused on urine for detection and monitoring of urological and other cancers. Other examples include cerebrospinal fluid for brain cancer, pleural fluid for lung cancer, peritoneal fluids for colorectal cancer, bile for biliary tract cancer, and uterine lavage for endometrial cancer.
Early-stage cancers tend to release very small amounts of ctDNA and other biomarkers into the blood, which also contains cell-free DNA (cfDNA) and other material derived from normal cells. Distinguishing tumor mutations from other genetic alterations present in blood cells can therefore pose challenges. On the other hand, non-blood-derived fluids that may be in direct contact with the tumor might contain higher levels of tumor-specific DNA and other biomarkers.
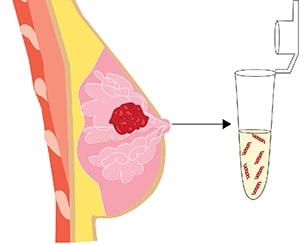
In a study that was recently published in the AACR journal Cancer Discovery, researchers focused their attention on breast milk. The analysis demonstrated that breast milk from 15 patients diagnosed with breast cancer while pregnant or breastfeeding contained higher levels of cfDNA than their blood, and that the integrity of the breast milk cfDNA was superior to that of blood cfDNA. Further, there was a higher prevalence of tumor DNA in breast milk compared with plasma.
The authors assessed matched tumor, breast milk, and blood samples for the presence of mutations in a set of genes that are frequently altered in the breast cancers of young patients. Mutations found in the tumor tissues were also detected in breast milk ctDNA in 13 patients but in blood ctDNA in only one patient.
Overall, breast milk analysis allowed for the detection of early-stage breast cancer with a 77.8% sensitivity. Comparing this result with previous liquid biopsy studies for breast cancer detection utilizing blood-derived ctDNA, the sensitivity of breast milk-derived tumor DNA genotyping was superior for both early and localized stages.
Strikingly, tumor-associated mutations were detected in the breast milk of two patients nine and 18 months before their cancers were diagnosed radiologically. These mutations were not detected in the breast milk of 12 age-matched healthy donors nor in milk samples derived from the patients’ unaffected breasts.
These findings indicate that breast milk liquid biopsy could be used as a tool for noninvasive early detection of breast cancer in a younger, lactating patient population that is typically excluded from breast cancer screening programs.
Another team investigated whether uterine fluid could be leveraged to detect ovarian cancer early, when the disease tends to be asymptomatic and most difficult to diagnose.
Since the ovarian surface, the fallopian tubes, and the uterine cavity form a communicating space, cancer cells and molecules secreted by ovarian tumors can flow into the uterine fluid. The investigators conducted a metabolomic analysis on uterine fluid samples collected from 96 individuals with early-stage and late-stage ovarian cancer, benign gynecological diseases, and endometrial cancer.
They identified a panel of seven metabolites that effectively distinguished patients with early ovarian cancer from those with late-stage ovarian cancer, benign gynecological disease, or endometrial cancer. The panel was validated in an independent set of uterine fluid samples from an additional 123 patients and had an area under the curve of 0.957. The investigators suggested that the panel performed better than the CA-125 test, which measures the amount of the protein CA-125 in the blood and can be used as a screening method in people with a high risk of developing ovarian cancer. This approach also allowed the researchers to characterize some of the metabolic changes that occur during ovarian cancer development.
The findings from these two studies, though preliminary, highlight the potential of body fluids beyond blood to be used for liquid biopsies for early cancer detection.



