Editors’ Picks: November Highlights from the AACR Journals
As the deep reds and yellows of fall leaves give way to twinkling holiday lights, we welcome the new season with a fresh selection of Editors’ Picks from the 10 AACR journals.
This month’s chosen articles include a possible way to prevent infections in patients receiving immunotherapy for multiple myeloma; a new set of potential biomarkers for Lynch syndrome-associated cancers; a mechanism by which fasting-mimicking diets may boost antitumor immunity; and much more. As always, these studies are freely available for a limited time.
Journal: Blood Cancer Discovery
BCMA-targeted bispecific antibodies (BiAb) are efficacious in relapsed/refractory multiple myeloma; however, serious infections have emerged as important toxicities. In this retrospective study, we characterized all infections and their risk factors, and evaluated the impact of infection prophylaxis in patients treated with BCMA-targeted BiAbs. Among 37 patients, 15 (41%) experienced a grade 3–5 infection, with two infection-related deaths during deep remissions. Most (84%) infections occurred during disease remissions. The cumulative probability of grade 3–5 infection increased over time with no plateau. Among responders (n = 26), profound hypogammaglobulinemia occurred in 100% and continued throughout the entire duration of treatment. During periods when patients were receiving intravenous immunoglobulin (IVIg), the rate of grade 3–5 infections was 90% lower than during observation (incidence rate ratio, 0.10; 95% confidence interval, 0.01–0.80; P = 0.0307). No other risk factors for infection were identified. This study demonstrates that profound hypogammaglobulinemia is universal with BCMA-targeted BiAbs, with intravenous immunoglobulin potentially abrogating most of the infection risk.
Significance: To the best of our knowledge, this is the first study to comprehensively analyze risk factors and mitigation strategies to prevent infections in myeloma patients receiving anti-BCMA bispecific antibodies. Profound and prolonged hypogammaglobulinemia was universal among responders, while immunoglobulin replacement was associated with 90% lower rates of grade 3–5 infections.
This study was highlighted and featured on the cover of the November issue. A related commentary on this article is available here, and an AACR press release is available here.
Journal: Cancer Discovery

We developed a phenotypic screening platform for the functional exploration of dendritic cells (DC). Here, we report a genome-wide CRISPR screen that revealed BCL2 as an endogenous inhibitor of DC function. Knockout of BCL2 enhanced DC antigen presentation and activation as well as the capacity of DCs to control tumors and to synergize with PD-1 blockade. The pharmacologic BCL2 inhibitors venetoclax and navitoclax phenocopied these effects and caused a cDC1-dependent regression of orthotopic lung cancers and fibrosarcomas. Thus, solid tumors failed to respond to BCL2 inhibition in mice constitutively devoid of cDC1, and this was reversed by the infusion of DCs. Moreover, cDC1 depletion reduced the therapeutic efficacy of BCL2 inhibitors alone or in combination with PD-1 blockade and treatment with venetoclax caused cDC1 activation, both in mice and in patients. In conclusion, genetic and pharmacologic BCL2 inhibition unveils a DC-specific immune checkpoint that restrains tumor immunosurveillance.
Significance: BCL2 inhibition improves the capacity of DCs to stimulate anticancer immunity and restrain cancer growth in an immunocompetent context but not in mice lacking cDC1 or mature T cells. This study indicates that BCL2 blockade can be used to sensitize solid cancers to PD-1/PD-L1–targeting immunotherapy.
This study was highlighted and featured on the cover of the November issue.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Long-term Cancer Survival Trends by Updated Summary Stage
Background: Stage is the most important prognostic factor for understanding cancer survival trends. Summary stage (SS) classifies cancer based on the extent of spread: In situ, Localized, Regional, or Distant. Continual updating of staging systems poses challenges to stage comparisons over time. We use a consistent summary stage classification and present survival trends for 25 cancer sites using the joinpoint survival (JPSurv) model.
Methods: We developed a modified summary stage variable, Long-Term Site-Specific Summary Stage, based on as consistent a definition as possible and applied it to a maximum number of diagnosis years, 1975–2019. We estimated trends by stage by applying JPSurv to relative survival data for 25 cancer sites in SEER-8, 1975–2018, followed through December 31, 2019. To help interpret survival trends, we report incidence and mortality trends using the joinpoint model.
Results: Five-year relative survival improved for nearly all sites and stages. Large improvements were observed for localized pancreatic cancer [4.25 percentage points annually, 2007–2012 (95% confidence interval, 3.40–5.10)], distant skin melanoma [2.15 percentage points annually, 2008–2018 (1.73–2.57)], and localized esophagus cancer [1.18 percentage points annually, 1975–2018 (1.11–1.26)].
Conclusions: This is the first analysis of survival trends by summary stage for multiple cancer sites. The largest survival increases were seen for cancers with a traditionally poor prognosis and no organized screening, which likely reflects clinical management advances.
Impact: Our study will be particularly useful for understanding the population-level impact of new treatments and identifying emerging trends in health disparities research.
This study was highlighted in the November issue.
Journal: Cancer Immunology Research
VISTA Expression on Cancer-Associated Endothelium Selectively Prevents T-cell Extravasation
Cancers evade T-cell immunity by several mechanisms such as secretion of anti-inflammatory cytokines, down regulation of antigen presentation machinery, upregulation of immune checkpoint molecules, and exclusion of T cells from tumor tissues. The distribution and function of immune checkpoint molecules on tumor cells and tumor-infiltrating leukocytes is well established, but less is known about their impact on intratumoral endothelial cells. Here, we demonstrated that V-domain Ig suppressor of T-cell activation (VISTA), a PD-L1 homolog, was highly expressed on endothelial cells in synovial sarcoma, subsets of different carcinomas, and immune-privileged tissues. We created an ex vivo model of the human vasculature and demonstrated that expression of VISTA on endothelial cells selectively prevented T-cell transmigration over endothelial layers under physiologic flow conditions, whereas it does not affect migration of other immune cell types. Furthermore, endothelial VISTA correlated with reduced infiltration of T cells and poor prognosis in metastatic synovial sarcoma. In endothelial cells, we detected VISTA on the plasma membrane and in recycling endosomes, and its expression was upregulated by cancer cell–secreted factors in a VEGF-A–dependent manner. Our study reveals that endothelial VISTA is upregulated by cancer-secreted factors and that it regulates T-cell accessibility to cancer and healthy tissues. This newly identified mechanism should be considered when using immunotherapeutic approaches aimed at unleashing T cell–mediated cancer immunity.
This study was featured on the cover of the November issue.
Journal: Cancer Prevention Research
Lynch syndrome (LS) markedly increases risks of colorectal and endometrial cancers. Early detection biomarkers for LS cancers could reduce the needs for invasive screening and surgical prophylaxis.
To validate a panel of methylated DNA markers (MDM) previously identified in sporadic colorectal cancer and endometrial cancer for discrimination of these cancers in LS.
In a case–control design, previously identified MDMs for the detection of colorectal cancer and endometrial cancer were assayed by qMSP on tissue-extracted DNA. Results were normalized to ACTB values within each sample. Least absolute shrinkage and selection operator models to classify colorectal cancer and endometrial cancer were trained on sporadic cases and controls and then applied to classify colorectal cancer and endometrial cancer, in those with LS, and cross-validated.
We identified colorectal cancer cases (23 with LS, 48 sporadic), colorectal controls (32 LS, 48 sporadic), endometrial cancer cases (30 LS, 48 sporadic), and endometrial controls (29 LS, 37 sporadic). A 3-MDM panel (LASS4, LRRC4, and PPP2R5C) classified LS-CRC from LS controls with an AUC of 0.92 (0.84–0.99); results were similar for sporadic colorectal cancer. A 6-MDM panel (SFMBT2, MPZ, CYTH2, DIDO1, chr10.4479, and EMX2OS) discriminated LS-EC from LS controls with an AUC of 0.92 (0.83–1.0); the AUC for sporadic endometrial cancer versus sporadic controls was nominally higher, 0.99 (0.96–1.0).
MDMs previously identified in sporadic endometrial cancer and colorectal cancer discriminate between endometrial cancer and benign endometrium and colorectal cancer and benign colorectum in LS. This supports the inclusion of patients with LS within future prospective clinical trials evaluating endometrial cancer and colorectal cancer MDMs and may provide a new avenue for cancer screening or surveillance in this high-risk population.
Prevention Relevance: Lynch syndrome (LS) markedly increases risks of colorectal and endometrial cancers. Early detection biomarkers for LS cancers could reduce the needs for invasive screening and surgery. Methylated DNA markers previously identified in sporadic endometrial cancer and colorectal cancer discriminate between benign and cancer tissue in LS.
This study was featured on the cover of the November issue.
Journal: Cancer Research (May 1 issue)
As a safe, feasible, and inexpensive dietary intervention, fasting-mimicking diet (FMD) exhibits excellent antitumor efficacy by regulating metabolism and boosting antitumor immunity. A better understanding of the specific mechanisms underlying the immunoregulatory functions of FMD could help improve and expand the clinical application of FMD-mediated immunotherapeutic strategies. In this study, we aimed to elucidate the role of metabolic reprogramming induced by FMD in activation of antitumor immunity against colorectal cancer. Single-cell RNA sequencing analysis of intratumoral immune cells revealed that tumor-infiltrating IgA+ B cells were significantly reduced by FMD treatment, leading to the activation of antitumor immunity and tumor regression in murine colorectal cancer models. Mechanistically, FMD delayed tumor growth by repressing B-cell class switching to IgA. Therefore, FMD-induced reduction of IgA+ B cells overcame the suppression of CD8+ T cells. The immunoregulatory and antitumor effects of FMD intervention were reversed by IgA+ B-cell transfer. Moreover, FMD boosted fatty acid oxidation (FAO) to trigger RUNX3 acetylation, thus inactivating Cα gene transcription and IgA class switching. IgA+ B-cell expansion was also impeded in patients placed on FMD, while B-cell expression of carnitine palmitoyl transferase 1A (CPT1A), the rate-limiting enzyme of FAO, was increased. Furthermore, CPT1A expression was negatively correlated with both IgA+ B cells and IgA secretion within colorectal cancer. Together, these results highlight that FMD holds great promise for treating colorectal cancer. Furthermore, the degree of IgA+ B cell infiltration and FAO-associated metabolic status are potential biomarkers for evaluating FMD efficacy.
Significance: Metabolic reprogramming of B cells induced by fasting-mimicking diet suppresses IgA class switching and production to activate antitumor immunity and inhibit tumor growth.
A commentary related to this study is available here.
Journal: Cancer Research (November 15 issue)
The ability of tumors to survive therapy reflects both cell-intrinsic and microenvironmental mechanisms. Across many cancers, including triple-negative breast cancer (TNBC), a high stroma/tumor ratio correlates with poor survival. In many contexts, this correlation can be explained by the direct reduction of therapy sensitivity induced by stroma-produced paracrine factors. We sought to explore whether this direct effect contributes to the link between stroma and poor responses to chemotherapies. In vitro studies with panels of TNBC cell line models and stromal isolates failed to detect a direct modulation of chemoresistance. At the same time, consistent with prior studies, fibroblast-produced secreted factors stimulated treatment-independent enhancement of tumor cell proliferation. Spatial analyses indicated that proximity to stroma is often associated with enhanced tumor cell proliferation in vivo. These observations suggested an indirect link between stroma and chemoresistance, where stroma-augmented proliferation potentiates the recovery of residual tumors between chemotherapy cycles. To evaluate this hypothesis, a spatial agent–based model of stroma impact on proliferation/death dynamics was developed that was quantitatively parameterized using inferences from histologic analyses and experimental studies. The model demonstrated that the observed enhancement of tumor cell proliferation within stroma-proximal niches could enable tumors to avoid elimination over multiple chemotherapy cycles. Therefore, this study supports the existence of an indirect mechanism of environment-mediated chemoresistance that might contribute to the negative correlation between stromal content and poor therapy outcomes.
Significance: Integration of experimental research with mathematical modeling reveals an indirect microenvironmental chemoresistance mechanism by which stromal cells stimulate breast cancer cell proliferation and highlights the importance of consideration of proliferation/death dynamics.
A commentary related to this study is available here.
Journal: Clinical Cancer Research (November 1 issue)
Purpose: This phase Ib study defined the safety, MTD, and recommended phase II dose (RP2D) of regorafenib combined with vincristine and irinotecan (VI). Secondary objectives were evaluation of antitumor activity and pharmacokinetics (PK) of regorafenib and irinotecan.
Patients and Methods: Patients aged 6 months to <18 years with relapsed/refractory solid malignancies [≥50% with rhabdomyosarcoma (RMS)] received regorafenib (starting dose 72 mg/m2/day) concomitantly or sequentially with vincristine 1.5 mg/m2 on days 1 and 8, and irinotecan 50 mg/m2 on days 1–5 (21-day cycle). Adverse events (AE) and tumor response were assessed. PK (regorafenib and irinotecan) were evaluated using a population PK model.
Results: We enrolled 21 patients [median age, 10 years; 12, RMS; 5, Ewing sarcoma (EWS)]. The MTD/RP2D of regorafenib in the sequential schedule was 82 mg/m2. The concomitant dosing schedule was discontinued because of dose-limiting toxicities in 2 of 2 patients treated. Most common grade 3/4 (>30% of patients) AEs were neutropenia, anemia, thrombocytopenia, and leukopenia. The overall response rate was 48% and disease control rate [complete response (CR)/partial response/stable disease/non-CR/non-progressive disease] was 86%. Median progression-free survival was 7.0 months [95% confidence interval (CI), 2.9–14.8] and median overall survival was 8.7 months (95% CI, 5.5–16.3). When combined with VI, regorafenib PK was similar to single-agent PK in children and adults (treated with regorafenib 160 mg/day).
Conclusions: Regorafenib can be combined sequentially with standard dose VI in pediatric patients with relapsed/refractory solid tumors with appropriate dose modifications. Clinical activity was observed in patients with RMS and EWS (ClinicalTrials.gov NCT02085148).
This article was highlighted in the November 1 issue.
Journal: Clinical Cancer Research (May 15 issue)
Purpose: This open-label, single-arm, phase II study evaluated the vascular endothelial growth factor receptor 2 (VEGFR2) tyrosine kinase inhibitor (TKI) rivoceranib in patients with recurrent or metastatic (R/M) adenoid cystic carcinoma (ACC).
Patients and Methods: Eligible patients had confirmed disease progression per Response Evaluation Criteria in Solid Tumors (RECIST) with ≥20% increase in radiologically or clinically measurable lesions or appearance of new lesions within the preceding 6 months. Patients received oral rivoceranib 700 mg once daily. Primary outcomes were objective response rate (ORR) by investigator review and by blinded independent review committee (BIRC).
Results: Eighty patients were enrolled and 72 were efficacy evaluable. Seventy-four patients had distant metastases and 49 received prior systemic treatment (14 received VEGFR TKIs). Per investigator and BIRC, respectively, ORR was 15.3% [95% confidence interval (95% CI), 7.9–25.7] and 9.7% (95% CI, 4.0–19.0); median duration of response was 14.9 months (95% CI, 4.9–17.3) and 7.2 months (95% CI, 3.5–8.4); and median progression-free survival was 9.0 months (95% CI, 7.3–11.5) and 9.0 months (95% CI, 7.7–11.5). Grade ≥3 treatment-related adverse events occurred in 56 patients (70.0%); the most common were hypertension (34, 42.5%) and stomatitis (6, 7.5%). Four grade 5 events occurred with one attributed to rivoceranib (epistaxis). Sixty-eight patients (85.0%) had ≥1 dose modifications and 16 patients (20.0%) discontinued rivoceranib for toxicity.
Conclusions: In patients with progressing R/M ACC, rivoceranib demonstrated antitumor activity and a manageable safety profile consistent with other VEGFR TKIs.
This article was highlighted in the November 15 issue.
Journal: Molecular Cancer Research
In this study, we identify USP1 as a transcriptional target of EWS::FLI1 and demonstrate the requisite function of USP1 in Ewing sarcoma (EWS) cell survival in response to endogenous replication stress. EWS::FLI1 oncogenic transcription factor drives most EWS, a pediatric bone cancer. EWS cells display elevated levels of R-loops and replication stress. The mechanism by which EWS cells override activation of apoptosis or cellular senescence in response to increased replication stress is not known. We show that USP1 is overexpressed in EWS and EWS::FLI1 regulates USP1 transcript levels. USP1 knockdown or inhibition arrests EWS cell growth and induces cell death by apoptosis. Mechanistically, USP1 regulates Survivin (BIRC5/API4) protein stability and the activation of caspase-9 and caspase-3/7 in response to endogenous replication stress. Notably, USP1 inhibition sensitizes cells to doxorubicin and etoposide treatment. Together, our study demonstrates that USP1 is regulated by EWS::FLI1, the USP1–Survivin axis promotes EWS cell survival, and USP1 inhibition sensitizes cells to standard of care chemotherapy.
Implications: High USP1 and replication stress levels driven by EWS::FLI1 transcription factor in EWS are vulnerabilities that can be exploited to improve existing treatment avenues and overcome drug resistance.
This study was highlighted in the November issue.
Journal: Molecular Cancer Therapeutics
Preclinical Development of Brain Permeable ERβ Agonist for the Treatment of Glioblastoma
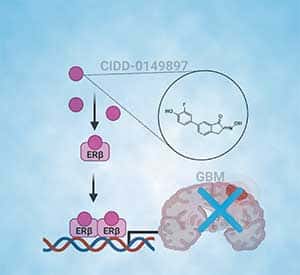
Glioblastoma (GBM) is the most prevalent and aggressive type of adult brain tumors with low 5-year overall survival rates. Epidemiologic data suggest that estrogen may decrease brain tumor growth, and estrogen receptor beta (ERβ) has been demonstrated to exert antitumor functions in GBM. The lack of potent, selective, and brain permeable ERβ agonist to promote its antitumor action is limiting the therapeutic promise of ERβ. In this study, we discovered that Indanone and tetralone-keto or hydroxyl oximes are a new class of ERβ agonists. Because of its high activity in ERβ reporter assays, specific binding to ERβ in polar screen assays, and potent growth inhibitory activity in GBM cells, CIDD-0149897 was discovered as a possible hit by screening a library of compounds. CIDD-0149897 is more selective for ERβ than ERα (40-fold). Treatment with CIDD-0149897 markedly reduced GBM cell viability with an IC50 of ∼7 to 15 μmol/L, while having little to no effect on ERβ-KO cells and normal human astrocytes. Further, CIDD-0149897 treatment enhanced expression of known ERβ target genes and promoted apoptosis in established and patient-derived GSC models. Pharmacokinetic studies confirmed that CIDD-0149897 has systemic exposure, and good bioavailability in the brain. Mice tolerated daily intraperitoneal treatment of CIDD-0149897 (50 mg/kg) with a 7-day repeat dosage with no toxicity. In addition, CIDD-0149897 treatment significantly decreased tumor growth in U251 xenograft model and extended the survival of orthotopic GBM tumor-bearing mice. Collectively, these findings pointed to CIDD-0149897 as a new class of ERβ agonist, offering patients with GBM a potential means of improving survival.
This article was highlighted and featured on the cover of the November issue.
Journal: Cancer Research Communications
Intraductal papillary mucinous neoplasms (IPMN) are cystic precursor lesions to pancreatic ductal adenocarcinoma (PDAC). IPMNs undergo multistep progression from low-grade (LG) to high-grade (HG) dysplasia, culminating in invasive neoplasia. While patterns of IPMN progression have been analyzed using multiregion sequencing for somatic mutations, there is no integrated assessment of molecular events, including copy-number alterations (CNA) and transcriptional changes that accompany IPMN progression. We performed laser capture microdissection on surgically resected IPMNs of varying grades of histologic dysplasia obtained from 23 patients, followed by whole-exome and whole-transcriptome sequencing. Overall, HG IPMNs displayed a significantly greater aneuploidy score than LG lesions, with chromosome 1q amplification being associated with HG progression and with cases that harbored co-occurring PDAC. Furthermore, the combined assessment of single-nucleotide variants (SNV) and CNAs identified both linear and branched evolutionary trajectories, underscoring the heterogeneity in the progression of LG lesions to HG and PDAC. At the transcriptome level, upregulation of MYC-regulated targets and downregulation of transcripts associated with the MHC class I antigen presentation machinery as well as pathways related to glycosylation were a common feature of progression to HG. In addition, the established PDAC transcriptional subtypes (basal-like and classical) were readily apparent within IPMNs. Taken together, this work emphasizes the role of 1q copy-number amplification as a putative biomarker of high-risk IPMNs, underscores the importance of immune evasion even in noninvasive precursor lesions, and reinforces that evolutionary pathways in IPMNs are heterogenous, comprised of both SNV and CNA-driven events.
Significance: Integrated molecular analysis of genomic and transcriptomic alterations in the multistep progression of IPMNs, which are bona fide precursors of pancreatic cancer, identifies features associated with progression of low-risk lesions to high-risk lesions and cancer, which might enable patient stratification and cancer interception strategies.