Dispelling Myths About Prostate Cancer in Black Communities
“The great enemy of truth is very often not the lie—deliberate, contrived, and dishonest, but the myth—persistent, persuasive, and unrealistic.” When John F. Kennedy delivered that remark, he wasn’t referring to prostate cancer, but his lesson applies nonetheless.
It is a fact that the incidence of prostate cancer is 60% higher in Black men compared to white men in the United States. But a common myth that if you feel fine then you don’t need a prostate exam may prevent people from getting screened.
It is a fact that Black men are 2.2 times more likely to die from prostate cancer than white men. But belief in the myth that prostate cancer is an old man’s disease—even though Black men are diagnosed at younger ages compared to white men—may make one put off screening until it is too late.
In a poster at the American Association for Cancer Research (AACR) Annual Meeting 2024, Mallorie C. Jones, MA, project manager, Division of General Internal Medicine in the Perelman School of Medicine at the University of Pennsylvania, presented a study in which she and her colleagues aimed to dispel myths like these by turning to a trustworthy member of the community—a Black pastor from Philadelphia who survived his own battle with prostate cancer.
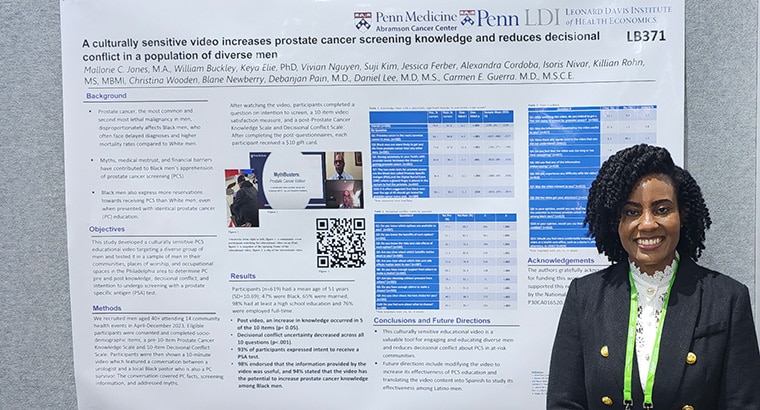
“Our study aimed to address these barriers by providing education from trustworthy and reliable sources in settings that were easily accessible to members of the community,” Jones explained in a press release.
They paired the pastor with a urologist over a video call and recorded their conversation to create a 10-minute educational resource that addresses both the facts and myths surrounding prostate cancer. Ultimately, the researchers found that 93% of those who watched the video said they would get screened. You can view a snippet from the video below.
Community Matters
To test the impact of the video, the researchers arranged 14 events between April and December 2023 within local Black communities at faith-based, union, and occupational spaces.
“We utilized a combination of indoor and outdoor events to maximize accessibility and visibility and collaborated with other specialties offering education, resources, or screenings whenever it was feasible,” Jones explained. “In addition to distributing the educational video and a survey, participants who completed the measures received giveaway items from the Philadelphia Flyers, the University of Pennsylvania, a $10 gift card, and the option to get a PSA screening by a licensed phlebotomist on-site.”
At these events, 619 men aged 40 and above agreed to watch the video and take part in the surveys. About half (47%) were Black men and the majority (98%) had at least a high school diploma. Of the 93% who said they would get screened after watching the video, Jones said they all did so on-site at the event. The phlebotomist drew a sample of their blood to test for amounts of the protein prostate-specific antigen—which is what PSA stands for—as high levels can be an indicator of prostate cancer.
Among those who didn’t get screened on-site, eight had a PSA screening recently and were not due for a retest. Another 10 participants said they had already scheduled or would schedule a screening with their own health care providers.
Raising Awareness
The participants were asked 10 questions pre- and post-video to assess their awareness about prostate cancer. After viewing the video, the researchers found an increase in knowledge for half of the questions, which touched on the following topics:
- Prostate cancer is the most common cancer in men.
- Black men are more likely to get and die from prostate cancer than any other men.
- A familial connection with prostate cancer increases the chance of developing the disease.
- The two main tests for prostate cancer are a PSA screening and a digital rectal exam, during which a gloved finger is placed in the rectum to feel the prostate.
- Black men over 40-years-old are recommended to get tested for prostate cancer every year.
Of those, Jones said one of their most important findings was that awareness of Black men’s higher propensity to get and die from this disease rose from 74% to 97%. Further, 98% indicated the information provided by the video was useful, 97% found the information credible, and 94% believed this resource could help increase awareness about prostate cancer among Black men.
For four of the questions, however, awareness did not significantly increase. These questions focused on whether:
- getting up to urinate at night was a sign of prostate cancer;
- a high-fat diet could decrease chances of developing the disease;
- just one of the screening methods would be enough; and
- early screening would not be able to tell if someone has prostate cancer.
“The length of the video may impact the ability of the participants to retain the entirety of the information,” Jones said in a press release. “We plan to amend the video to contain a brief recap to reinforce all of the items that were asked about on the knowledge questionnaire, but with an emphasis on those that did not yield a statistically significant post-video result.”
In the future, once Jones and her colleagues optimize the video to maximize its effectiveness and have published the study, they hope to share it so it can be used as an educational resource. For instance, Jones said the video could be used by unions such as Local 22 of the International Association of Fire Fighters, which represents Philadelphia firefighters and paramedics, and the American Federation of Labor and Congress of Industrial Organizations (AFL-CIO), which represents more than 12.5 million working people.
They also would like to collaborate with community organizations that have greater access to Black men—such as local chapters of the National Association for the Advancement of Colored People (NAACP)—or those with perceived environmental and/or occupational predispositions to cancer. They intend to explore ways to make this type of information more accessible to Spanish-speaking individuals, as well.
“Not only may this culturally sensitive educational video be a valuable asset when educating diverse groups of men about prostate cancer and prostate cancer screening,” Jones said, “but this may also be a useful technique that can be applied to a variety of topics and populations.”