FDA Approvals in Oncology: October-December 2025
Science faced many obstacles in 2025, but that didn’t stop the advances from coming. Over the course of the year, the U.S. Food and Drug Administration (FDA) issued more than 50 approvals in oncology, with 20 of these coming in just the final three months.
You can read about the approvals from January through September in our previous blog posts:
- FDA Approvals in Oncology: January-March 2025
- FDA Approvals in Oncology: April-June 2025
- FDA Approvals in Oncology: July-September 2025
And keep scrolling for a roundup of the FDA approvals from the year’s final quarter and insights into how these fit into the therapeutic landscape.
Expanded Use for Menin Inhibitors
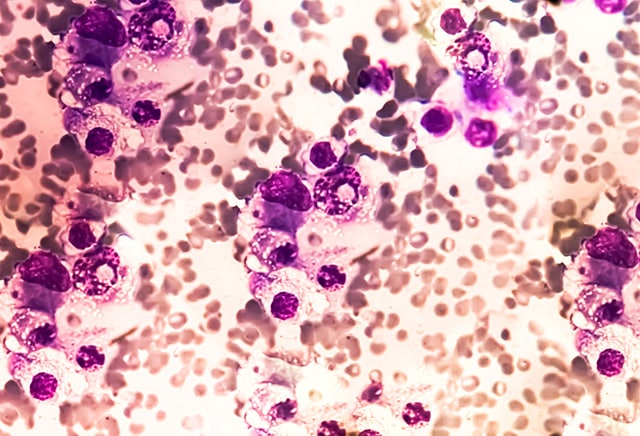
It was just over a year ago that the FDA approved revumenib (Revuforj), the first inhibitor of the menin protein, which forms a complex with the mixed lineage leukemia 1 (MLL1) protein to mediate cancer-promoting gene expression.
Now, menin inhibitors are back in the roundup, with a new indication for revumenib and the approval of a second menin inhibitor.
- Revumenib’s approval was expanded to include patients 1 year of age or older who have relapsed or refractory acute myeloid leukemia (AML) that harbors a susceptible nucleophosmin 1 (NPM1) mutation and who have no satisfactory alternative treatment options.
- Ziftomenib (Komzifti) was approved for adult patients with relapsed or refractory AML with a susceptible NPM1 mutation who have no satisfactory alternative treatment options. This is the first FDA approval for ziftomenib.
Mutated forms of NPM1, found in many cases of AML, can enhance oncogenic gene expression by binding to the menin-MLL1 complex, according to a study published in Cancer Discovery, an American Association for Cancer Research (AACR) journal.
First Approved Treatment for Smoldering Multiple Myeloma
Smoldering multiple myeloma is an asymptomatic, slow-growing condition that can progress to active multiple myeloma. It has traditionally been managed with active monitoring, but a new treatment approved last quarter provides the first intervention that might slow its progression to active multiple myeloma.
- Daratumumab and hyaluronidase (Darzalex Faspro) was approved as a monotherapy for adults with high-risk smoldering multiple myeloma.
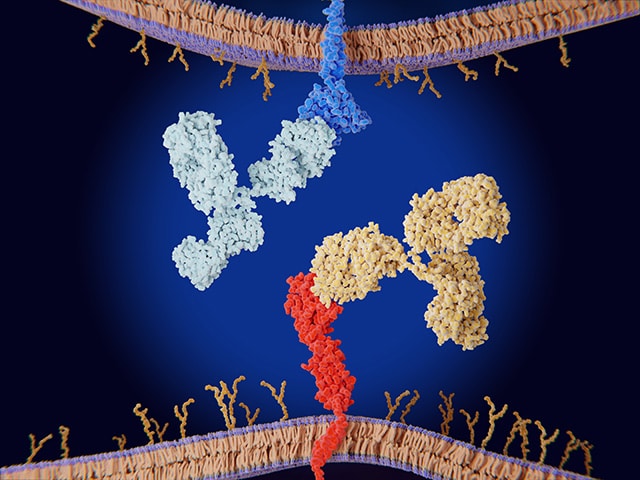
Daratumumab is a monoclonal antibody that binds to the protein CD38, which is highly expressed on the surface of abnormal plasma blood cells, such as those that comprise multiple myeloma. Binding of daratumumab to CD38 leads to cell death. The hyaluronidase element of the treatment allows daratumumab to be administered subcutaneously by partially breaking down the extracellular matrix around cells so that daratumumab can reach CD38-expressing cells more effectively.
Expanded Approvals for Antibody-drug Conjugates
During the final three months of 2025, the FDA approved new indications for two antibody-drug conjugates (ADCs). These targeted therapeutics are comprised of a cytotoxic agent in complex with an antibody that targets a cancer-associated protein. ADCs selectively bind to cells that express the target protein and release the cytotoxic agent inside these cells to kill them.
- Trastuzumab deruxtecan (T-DXd; Enhertu) was approved in combination with pertuzumab (Perjeta) as a first-line treatment for unresectable or metastatic, human epidermal growth factor receptor 2 (HER2)-positive breast cancer. T-DXd selectively binds to cells expressing the HER2 protein, which promotes cell growth that can fuel cancer progression.
The expanded indication allows T-DXd—which was previously approved for the second-line or later setting—to be given to patients who have not yet received treatment. A panel of experts discussed clinical considerations for first-line use of T-DXd at the recent San Antonio Breast Cancer Symposium; their discussion was summarized in a recent blog post. - Belantamab mafodotin (Blenrep) was approved in combination with bortezomib (Velcade) and dexamethasone for patients with relapsed or refractory multiple myeloma after at least two prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent.
Belantamab mafodotin targets the B-cell maturation antigen (BCMA) protein, which is preferentially expressed on mature B cells, including multiple myeloma cells. This ADC was previously granted an accelerated approval as a monotherapy for certain relapsed or refractory multiple myelomas, but that approval was later withdrawn following clinical trial findings that showed it was no better than existing treatments. The new approval is based on results that demonstrated the superiority of the belantamab mafodotin-containing combination compared with standard treatment.
New Treatment Options for Lung Cancer
Lung cancer is one of the most commonly diagnosed forms of cancer in the United States, and during 2025’s last quarter, two therapeutics were approved to treat different forms of lung cancer.

- Lurbinectedin (Zepzelca) was approved in combination with the immune checkpoint inhibitor atezolizumab (Tecentriq or Tecentriq Hybreza) for the maintenance treatment of extensive-stage small cell lung cancers (ES-SCLCs) that have not progressed following first-line induction therapy.
Small cell lung cancers are typically fast-growing, and extensive-stage cancers are those that have spread to other parts of the body. Lurbinectedin is a DNA-damaging agent and was previously approved to treat ES-SCLCs that had progressed after first-line therapy. The new approval makes it available earlier, before disease progression. - Sevabertinib (Hyrnuo), a small-molecular inhibitor of HER2, received accelerated approval to treat patients with advanced non-small cell lung cancers (NSCLC) that harbor activating mutations in HER2 and who have been previously treated with systemic therapy. Approximately 2% to 4% of NSCLCs harbor such mutations.
Sevabertinib is the second small-molecule HER2 inhibitor approved for this patient population, following the August 2025 approval of zongertinib (Hernexeos) for previously treated, advanced NSCLC with HER2-activating mutations. These two HER2 inhibitors are administered orally and do not inhibit the wild-type form of the epidermal growth factor receptor (EGFR), potentially reducing the risk of severe side effects associated with T-DXd, which is also approved for NSCLC.
The preclinical activity of sevabertinib, which is a reversible dual EGFR-HER2 inhibitor, was published in Cancer Discovery, an AACR journal, along with early results from the clinical trial that ultimately led to its accelerated approval.
MEK Inhibitor Approval Expanded to Include Adults
Last quarter, the FDA expanded the approval of selumetinib, a MEK inhibitor previously approved for children, to include certain adult patients.
- Selumetinib (Koselugo) was approved for adults with neurofibromatosis type 1 (NF1) with symptomatic, inoperable plexiform neurofibromas (PN).
Although they are typically benign, plexiform neurofibromas can cause substantial clinical complications, including chronic pain and functional impairment. In some cases, these benign tumors can become malignant. MEK1 and MEK2 are proteins within the MAPK signaling pathway, which regulates cell growth, differentiation, and survival. Activating mutations in MEK proteins can lead to aberrant activation of the MAPK pathway and uncontrolled cell growth. By targeting MEK, selumetinib disrupts this tumor-promoting signaling.
First PARP Inhibitor for Castration-sensitive Prostate Cancer
Mutations in BRCA1/2 or other proteins in the homologous recombination (HR) pathway—which repairs damaged DNA—are found in approximately one-quarter of metastatic prostate cancers. While these mutations are associated with poor prognosis, they also make prostate cancer cells susceptible to PARP inhibitors, which kill HR-mutated cells through synthetic lethality.
Multiple PARP inhibitors have been approved for HR-mutated metastatic castration-resistant prostate cancer (mCRPC), and last quarter, the FDA issued the first approval of a PARP inhibitor for HR-mutated metastatic prostate cancers that are still sensitive to androgen-reducing interventions.
- Niraparib and abiraterone acetate (Akeega) in combination with prednisone was approved this quarter for patients with metastatic castration-sensitive prostate cancers with deleterious or suspected deleterious BRCA2 mutations.
Niraparib is a PARP inhibitor, abiraterone acetate is a hormone therapy that blocks the production of testosterone, and prednisone is a steroid that can mitigate treatment side effects. This regimen was previously approved for BRCA1/2-mutated mCRPC.
New Indications for Immunotherapies
Immunotherapy is a class of cancer therapy that exploits the intrinsic ability of the immune system to attack cancer cells. Different forms of immunotherapy boost antitumor immune activity in various ways, and last quarter, the FDA issued new indications for three immune checkpoint inhibitors, one cell-based immunotherapy, and one T-cell engager.
- Cemiplimab (Libtayo) was approved for use after surgery and adjuvant radiation in patients whose cutaneous squamous cell carcinoma (CSCC)—one of the most common forms of skin cancer—has a high risk of recurring. Cemiplimab is an immune checkpoint inhibitor that reverses the brakes on T cells by binding to the PD-1 protein on T cells. Binding of cemiplimab to PD-1 prevents PD-1 from interacting with its ligand, PD-L1, on cancer and other cells to suppress T-cell activity.
The FDA previously approved cemiplimab for patients with advanced cases of CSCC who are not eligible for surgery and radiation. The latest approval allows cemiplimab to be used in patients with earlier stages of CSCC who are eligible for these treatments. It is the first adjuvant immunotherapeutic approved to help prevent the recurrence of high-risk CSCC. - The FDA also approved pembrolizumab (Keytruda)—another PD-1-targeted immune checkpoint inhibitor—in combination with the Nectin-4-directed ADC enfortumab vedotin (Padcev) as neoadjuvant and adjuvant treatment for patients with muscle-invasive bladder cancer who are ineligible to receive cisplatin.
This combination regimen was previously approved for patients with advanced muscle-invasive bladder cancers, and the latest approval makes it available for earlier-stage cases as well.
- Durvalumab (Imfinzi) plus chemotherapy was approved for neoadjuvant and adjuvant treatment, followed by durvalumab monotherapy, for the treatment of resectable gastric or gastroesophageal junction adenocarcinoma. Durvalumab is another immune checkpoint inhibitor, but unlike cemiplimab and pembrolizumab, it works by binding to PD-L1 instead of to PD-1. This is durvalumab’s first approval for this cancer type.
- Lisocabtagene maraleucel (Breyanzi) was approved to treat patients with relapsed or refractory marginal zone lymphomas after two or more prior lines of systemic therapy. Lisocabtagene maraleucel is a chimeric antigen receptor (CAR) T-cell therapy, a type of cell-based immunotherapy in which a patient’s T cells are isolated from blood, engineered to recognize and attack cancer cells, and infused back into the patient’s body.
While lisocabtagene maraleucel has been approved for various other forms of lymphoma, this is its first approval for marginal zone lymphoma, a rare and slow-growing type of lymphoma. The approval marks the first CAR T-cell therapy approved for this cancer type. - Epcoritamab (Epkinly) was approved in combination with lenalidomide (Revlimid) and rituximab (Rituxan) to treat relapsed or refractory follicular lymphoma. Epcoritamab is a bispecific antibody, a type of immunotherapy designed to bring cancer-fighting T cells into proximity with cancer cells. It does so by simultaneously binding to the protein CD20 on B cells (the cell type from which follicular lymphoma arises) and the CD3 protein on T cells.
Biosimilars and New Formulations
The FDA also approved alternate versions of existing drugs to give patients more choices with their treatment.
- Pertuzumab-dpzb (Poherdy) was approved as the first biosimilar to pertuzumab, providing patients with a potentially less expensive alternative to this common breast cancer treatment.
Pertuzumab-dpzb can be used interchangeably with pertuzumab to treat certain adults with HER2-positive breast cancer because their structures and activity are highly similar with no clinically meaningful differences in safety or efficacy. Both drugs are monoclonal antibodies that target HER2 to disrupt critical cell signaling and induce cell death. - Amivantamab and hyaluronidase (Rybrevant Faspro) is a newly approved formulation of amivantamab (Rybrevant) that allows the therapeutic to be delivered via subcutaneous injection instead of intravenously. The subcutaneous formulation may be used for all indications for which the intravenous formulation is approved.
Amivantamab inhibits the activity of the EGFR and MET proteins and has been approved to treat certain EGFR-mutated lung cancers. Early clinical trial results supporting the safety of subcutaneously delivered amivantamab were reported at the AACR Annual Meeting 2022.
Conversions of Accelerated Approvals to Traditional Approvals
The FDA’s Accelerated Approval Program allows treatments to receive accelerated approval based on surrogate endpoints that can provide early support for a treatment’s efficacy. The accelerated approval may be converted to a traditional approval if follow-up clinical testing confirms that the treatment provides clinical benefit.
Last quarter, the FDA converted several accelerated approvals to traditional approvals based on confirmatory clinical trial results. These included:
- epcoritamab monotherapy for patients with relapsed or refractory follicular lymphoma who have received at least two lines of systemic therapy;
- daratumumab and hyaluronidase with bortezomib, cyclophosphamide, and dexamethasone for the first-line treatment of light-chain amyloidosis, a potentially fatal condition that can occur in patients with multiple myeloma;
- pirtobrutinib (Jaypirca) for patients with relapsed or refractory chronic lymphocytic leukemia or small lymphocytic lymphoma who have received prior treatment with another inhibitor of Bruton’s tyrosine kinase;
- tarlatamab (Imdelltra) for patients with ES-SCLC whose disease progressed during or after platinum-based chemotherapy; and
- rucaparib (Rubraca) for patients with BRCA-mutated mCRPC that has been treated with androgen receptor-directed therapy.
Check out our FDA approvals page for a comprehensive overview of each oncology approval, including the clinical data that led to each.



