Sentinels of the Lung: Alveolar Macrophages and Cancer Onset
The diversity of the tumor macrophage compartment remains to be fully understood – a potential opportunity for therapeutic strategy development. Maria Casanova-Acebes, PhD, and her research colleagues reported that tissue-resident macrophages (TRMs) were located in close proximity to tumor cells during early lung cancer development (1). Furthermore, they showed that these TRMs promoted tumor cell epithelial-mesenchymal transition, migration, and invasiveness, presenting a therapeutic opportunity that may be exploited for lung cancer interception.
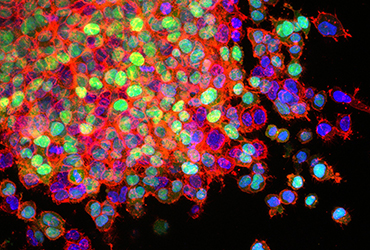
Lung Cancer Metastasis. Source: National Cancer Institute \ Winship Cancer Institute of Emory University
Describing their work, Dr. Casanova-Acebes says, “The prevailing dogma was that solid tumors were mainly populated by bone marrow-derived macrophages. Our work identified many macrophage classes in lung tumors, way more than the classic M1-M2 subtypes. We observed that macrophages also change upon tumor progression and this implies that we will need to design better strategies that aim to reprogram or target macrophages, taking this dynamic behavior into consideration.”
In her recently published work in Nature, she and her colleagues reported on the distinct molecular signature of tissue-resident macrophages (TRMs) (referred to as alveolar macrophages in the case of lung cancer). In particular, these TRMs underwent transcriptional changes in genes related to antigen presentation and tissue remodeling in response to tumor seeding. Conversely, the presence of the TRMs impacted tumor cell gene expression, especially of genes associated with migration, epithelial-mesenchymal transition and lipid metabolism. Transwell assay results confirmed the increased migratory ability of tumor cells that had been cultured in TRM conditioned medium. In addition, 3D matrigel assays showed that tumor cells cultured with TRMs formed invasive protrusions, while those cultured with tumor-associated monocyte-derived macrophages or bone marrow monocytes did not.
Previous work from Dr. Merad’s research group, where Dr. Casanova-Acebes was a Fellow, had shown that Tregs are significantly increased in lung tumor tissue vs in normal lung tissue (2). In this current work, they confirmed increased Treg proliferation in early tumor lesions. Imaging of these early tumors showed that these Tregs were in close proximity to TRMs. Depleting TRMs in a mouse model reduced the number of Tregs in early lung cancer lesions without affecting Treg numbers in tumor-draining lymph nodes or the spleen. Moreover, depletion of TRMs in early-stage lesions reduced the size of tumors without affecting the number of tumor lesions. In contrast, depletion of TRMs in established tumor lesions did not affect tumor burden.
Dr. Casanova-Acebes received an AACR-AstraZeneca Immuno-oncology Fellowship in 2020 at the Icahn School of Medicine at Mount Sinai. With the support of the AACR-AstraZeneca fellowship and mentorship by Miriam Merad, MD, PhD, she sought to elucidate the contribution of tissue-resident macrophages in lung adenocarcinoma. Dr. Acebes is now head of the Cancer Immunity Group at the Spanish National Cancer Research Centre (CNIO).
Highlighting the impact of AACR grant support on her career, she shares, “Being an awardee of the AACR grants program fostered my career enormously. I got to know many cancer biologists through the AACR grantee club meetings. These meetings were of enormous help in establishing new collaborations across the oceans. It also helped my research to continue going, even beyond the grant end date. Being an AACR awardee has also helped me to connect to other disciplines in cancer research. i.e. beyond immunology, thereby opening new horizons in my program to explore in the upcoming years.”
References:
- Casanova-Acebes M, Dalla E, Leader AM, LeBerichel J, Nikolic J, Morales BM, et al. Tissue-resident macrophages provide a pro-tumorigenic niche to early NSCLC cells. Nature 2021; 595: 578–584
- Lavin Y, Kobayashi S, Leader A, Amir ED, Elefant N, Bigenwald C, et al. Innate Immune Landscape in Early Lung Adenocarcinoma by Paired Single-Cell Analyses. Cell 2017; 169:750-765