AACR Past President Leads Important Conversations on Screening, Prevention
Monday afternoon, First Lady Jill Biden visited the Medical University of South Carolina (MUSC) Hollings Cancer Center as part of Breast Cancer Awareness Month. Staffers and patient advocates told Biden about several initiatives that have aimed to reduce racial disparities in breast cancer outcomes, from a partnership with a historically Black university to a mobile health unit that has brought breast cancer screening to 25,000 women since 2009.

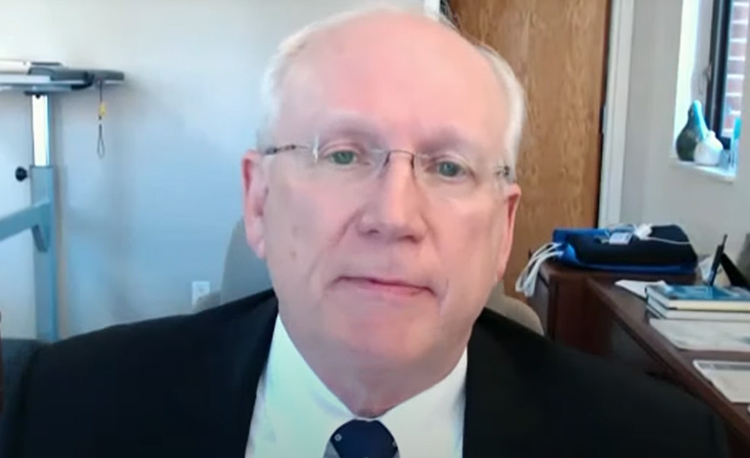
Biden’s host: Raymond N. DuBois, MD, PhD, FAACR, a Past President of the American Association for Cancer Research (AACR). DuBois currently serves as Dean of the College of Medicine at MUSC and is Director of the MUSC Hollings Cancer Center, and as Chair and President of the AACR Foundation.
Monday’s visit with Biden continued a busy week of advocacy for DuBois. On Wednesday, October 20, he testified on behalf of the AACR before the House Energy and Commerce Subcommittee on Health. During a hearing titled “Enhancing Public Health: Legislation to Protect Children and Families,” DuBois discussed the evolving science and importance of cancer screenings. He highlighted how cancer organizations such as the AACR publish research that informs decisions on appropriate types and levels of cancer screening and discussed how emerging research in cancer prevention and treatment will benefit public health.
DuBois is also the Editor-in-Chief of the AACR journal Cancer Prevention Research, which published a commentary from DuBois based on his testimony on this critical topic.
Here is the full text:
Chairwoman Eshoo, Ranking Member Guthrie, and members of the subcommittee, thank you for inviting me today … I commend you for holding this hearing to discuss the importance of cancer prevention for public health and I am very pleased that you’re including cancer screenings as part of these discussions.
Research Behind Cancer Screening
The data show that cancer screenings save lives and improve outcomes because cancers and pre-cancers can be identified at an earlier stage, when physicians can treat it much more effectively. This often results in less invasive treatment, quicker recovery, and a lower cost.
Cancer organizations such as the AACR publish research that informs the medical community about developments on who, and how, to most effectively screen for different types of cancer. The most influential body is the U.S. Preventive Services Task Force, or USPSTF, which examines the evidence of lower cancer mortality as well as potential risks, such as costs, false negatives and positives, and complications of follow-up procedures in order to generate screening guidelines. Under the Affordable Care Act, those screening tools graded with an A or a B are required to be covered by insurance without cost to the patient.
As more research is generated, the USPSTF can update its guidelines. This year, the USPSTF broadened eligibility for lung cancer and colon cancer screenings. For lung cancer, after reviewing clinical trial results that found screening a larger segment of the smoking population decreased lung cancer deaths by 24 percent after 10 years, the USPSTF expanded screening eligibility to smokers as young as 50 who smoked a pack a day for 20 years, nearly doubling the number of individuals who can now be screened at no cost. Previously, only older Americans who smoked a pack a day for 30 years were eligible. These new guidelines are especially beneficial for women and African Americans, who tend to smoke fewer cigarettes than white men yet still have a high risk of developing lung cancer.
The USPSTF also reduced the age recommendations for colonoscopies from 50 to 45, after reviewing evidence of an increase in colon cancer diagnoses among middle-aged Americans.
Ensuring Screening Is Available for At-risk Populations
I am of the strong belief that effective screening is much better than no screening. However, that does not mean that screening for all cancers without a scientific basis to do so is in the public interest. Overscreening can be cost- prohibitive and comes with side effects including radiation exposure and other complications.
The USPSTF has to balance the evidence and the risks vs. benefits. Policymakers should be mindful of USPSTF recommendations and evolving science, as well as other items that should be considered. For lung cancer, for example, the USPSTF recommends screening based on smoking history and age, but does not take into account whether a person grew up in a home with smokers and may have had substantial exposures to secondhand smoke, or increased risk due to occupation or environmental factors. Colon cancer screenings do not take into account the growing evidence that younger obese Americans are being diagnosed with colon cancer at an increasing rate. Mammograms have a high false-positive rate which can lead to unnecessary biopsies and added stress, but a recommendation to start mammograms for women at age 50 will leave many younger women vulnerable for breast cancer that could spread before it would have been detected.
I’d encourage Congress to consider the impact on the individual rather than on the broader population. When designing screening criteria, Congress and the USPSTF should consider heightened cancer risk factors among underserved populations, such as occupation, environmental exposure, and lifestyle factors. Simple age-based criteria contribute to inequities experienced by underserved communities and demographics underrepresented in screening trials. We need to ensure that all racial and ethnic groups and socioeconomic classes have the knowledge to make informed decisions as well as access to evidence-based screening and, importantly, affordable follow-up for positive screens.
In South Carolina, the incidence of breast cancer in Black women is lower than in White women, but Black women’s death rate is higher because they have longer delays before they get screened and treated, potentially due to lack of access to health services, mistrust in the health care system, and diagnostic failure.
The mortality rate of prostate cancer in Black men is much worse than white men, and while there could be genetic influences, it is most likely due to lack of access to specialty care and health facilities. These disparities highlight a real and growing threat to public health.
Screening and treatment outcome disparities are areas in which the medical research community must improve. Medicaid expansion would play a significant role in reducing these health disparities, and the scientific research community must continue to study the most successful methods for cancer screening, particularly for hard to detect cancers such as pancreatic, ovarian, and brain cancers, which currently lack any screening option.
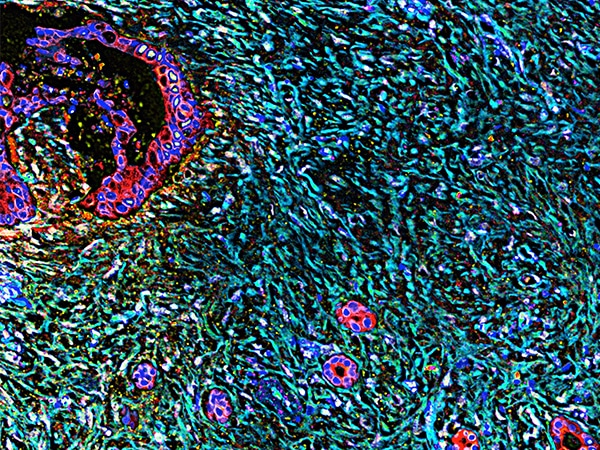
The medical community can also bring new tools to at-risk communities. At the MUSC Hollings Cancer Center, we are working to reduce the cancer burden in the I-95 Corridor region. This area, stretching from Georgia to North Carolina, is largely rural and economically disadvantaged, and the majority of the population are in older minority communities. If you look at a map of cancer deaths in South Carolina, it looks like a heat map of this region lighting up.
Hollings Cancer Center has established Mobile Health Units that travel to underserved areas and work with community health centers, churches, community centers, and employers to bring cancer screening to the people who need it the most.
Future of Cancer Screening
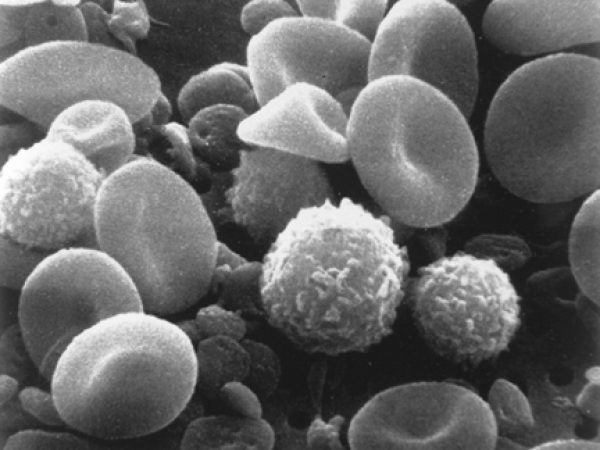
In addition to advances in health care delivery, thanks to congressional investment in basic and translational research, we are at an exciting time in cancer screening. Several academic institutions and industry are making progress on a pan-cancer blood test that would detect certain cancers with very high sensitivity. Cancer in your body sheds a DNA signature into the blood, and these emerging blood tests can detect whether cancer is present and what type of cells the DNA came from. Once validated and proven, these less invasive tests could greatly expand access while reducing costs.
COVID-19 and Cancer Screening
Before I conclude, it’s important to mention that we are still not yet at pre-pandemic levels for cancer screening. The National Cancer Institute estimates that due to COVID-19 delaying cancer screenings, as many as 10,000 additional Americans could die of breast and colon cancer alone in the coming decade. As the scientific community works to improve cancer screening, it is imperative that individuals still maintain recommended screenings from their health providers. The earlier we can detect cancers, the better chance a patient has for living a longer, healthier life.
The AACR welcomes the opportunity to serve as a resource as you develop these proposals. Our recently released AACR Cancer Progress Report 2021 also includes up-to-date information on developments in cancer screenings, treatment, and care, and is available on our website.
Thank you again for the opportunity to testify before you today.