Driving Progress Against RAS-driven Cancers
Outside the lab, Frank McCormick, PhD, FAACR, is a racecar driver, nurturing a passion he developed decades ago. (“We all need hobbies, right?” he says with a grin.)
Inside the lab, he uses a similar passion to understand a more insidious type of driver—proteins that cause cancer.
Among the cancer drivers studied by McCormick are the RAS family of proteins, the first of which was identified and isolated by Mariano Barbacid, PhD, FAACR, and others in 1982, just one of a series of seminal discoveries that led Nature to dub 1982 “The Year of the Oncogene.”
In the 40+ years since, immense progress has been made in understanding how RAS proteins contribute to cancer and how they might be therapeutically targeted. Ten years ago, Kevan Shokat, PhD, and colleagues published a revolutionary study that opened the possibility for directly targeting mutant KRAS. Today, two direct inhibitors of the KRASG12C mutant are approved to treat patients with lung cancer, a feat once considered unattainable.
“The whole field has exploded in the last four or five years,” said McCormick in an interview with Cancer Research Catalyst. McCormick served as the 2012-2013 President of the AACR.

“The most exciting area really is the development of drugs that target KRAS directly. It’s [been] 10 years since the first ideas were published showing how that could be done, but now we have lots of other [investigational] drugs … using different approaches,” he said.
Despite immense strides in treating RAS-driven cancers, there is still much work to be done. McCormick notes that overcoming treatment resistance and developing clinically effective methods to target different KRAS mutants are key priorities.
“We need a battery of different drugs. The more potent the drugs, all the better in terms of reducing the frequency of resistance,” he said. “We need drugs that target the resistant forms that emerge, downstream pathways, and indirect approaches, such as harnessing the immune system, shutting down some of the effects of stromal cells, and other orthogonal approaches.”
Similarly, Barbacid contends that the future of treating KRAS-mutated cancers will rely on developing direct inhibitors of other mutant isoforms of KRAS, such as the KRASG12D and KRASG12V isoforms common in pancreatic cancers, and targeting signaling downstream of KRAS, which would be effective against all KRAS isoforms.
McCormick, Barbacid, and other researchers from around the world gathered in Philadelphia for the AACR Special Conference: Targeting RAS to discuss the past, present, and future of treating RAS-driven cancers.
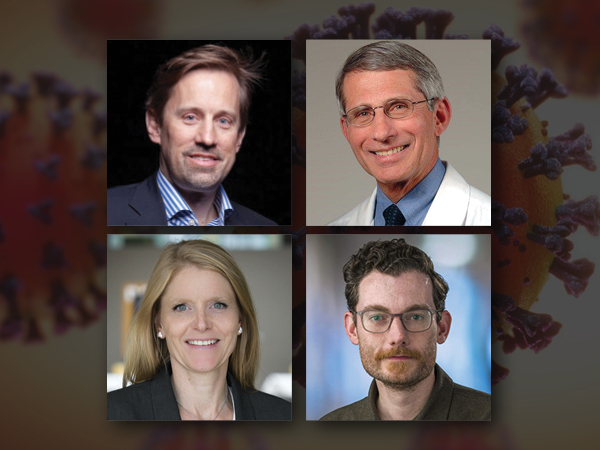
The meeting was held March 5-8 and organized by McCormick (University of California, San Francisco); Barbacid (Centro Nacional de Investigaciones Oncológicas in Madrid); Dafna Bar-Sagi, PhD, FAACR (NYU Langone Health); and Deborah Morrison, PhD (National Cancer Institute of the National Institutes of Health).
As described by McCormick, the meeting served as an update on the “enormous” progress in developing new ways to target RAS, with a focus on “how these drugs behave in the clinic, how patients develop resistance, how we can overcome resistance, and how we can combine these drugs with other types of drugs to improve patient benefit.”
With a meeting like this, he notes, “there’s always unexpected new scientific breakthroughs that change the direction of the field and take us in new areas we hadn’t thought of previously.”
Opening Keynote Reveals Novel Triple Therapy Approach to Overcome Treatment Resistance
Barbacid welcomed conference attendees with a keynote lecture on understanding and circumventing resistance to KRAS inhibition. Using various mouse models, he and colleagues identified changes in drug metabolism and amplification of the KRAS gene—rather than additional mutations in KRAS—as potential mechanisms of treatment resistance.

In the second half of his lecture, he shared a novel approach to turn off signaling downstream of oncogenic KRAS. Efforts to target many downstream MAPK signaling proteins have been hindered by unacceptable toxicity, he explained, but recent research from his group demonstrated that combined targeting of RAF1 and EGFR might be a feasible strategy. Now, he and colleagues have found that simultaneously targeting a third protein—STAT3—might improve responses. The experiments were performed in cell and mouse models in which the RAF1, EGFR, and STAT3 genes were all deleted. In these models, cancer cells that were unresponsive to RAF1 and EGFR ablation responded to the triple gene ablation, although there was some toxicity associated with STAT3 deletion.
A STAT3-targeted proteolysis targeting chimera (PROTAC) developed by Barbacid and colleagues has shown some promising early results in preclinical experiments. Moving forward, they hope to identify a pharmacologic strategy to selectively degrade RAF1 as well, with the ultimate goal of testing these molecules in combination with an existing EGFR inhibitor, such as erlotinib (Tarceva) or gefitinib (Iressa). Barbacid added that combining the triple therapy strategy with a direct KRAS inhibitor is another approach he is interested in pursuing.
Rising Star Lecture Highlights Cell State Changes as a Targetable Resistance Mechanism
Barbacid’s presentation was followed by one from Andrew Aguirre, MD, PhD, who was awarded the distinction of “Rising Star” by the meeting organizers. Aguirre is a medical oncologist at Dana-Farber Cancer Institute, an associate professor at Harvard Medical School, and an associate member of the Broad Institute of Harvard and MIT.
“It’s so important to bring new people into the field so that we can really learn more from fresh new ideas,” said Bar-Sagi as she invited Aguirre to the podium.
MD, PhD
Aguirre shared data illustrating how resistance to KRAS inhibitors can develop through changes in cell state, independently of genetic alterations. In a lung adenocarcinoma cell line, overexpression of the ΔNp63 squamous cell marker led to resistance to a KRAS inhibitor, suggesting that transition from an adenocarcinoma cell state to a squamous cell state may be involved in treatment resistance. Results from mouse and organoid studies supported the association of adeno-squamous transition with treatment resistance.
Furthermore, a retrospective analysis showed that patients whose tumors expressed a squamous cell gene signature at baseline had been treated with the KRAS inhibitor adagrasib for less time than those without the signature, a sign that the tumors with squamous cell markers may have stopped responding to the treatment earlier. Aguirre acknowledged that a limitation of their analysis is that patients may have stopped treatment for other reasons as well.
Nonetheless, he is excited about the potential of targeting cell state transition as an approach to prevent or overcome resistance to KRAS inhibition.
For the final portion of his presentation, Aguirre spoke of the “enormous potential” of RAS-targeted therapies, highlighting some of the therapeutic strategies under investigation. Treating patients with a KRAS inhibitor during earlier lines of treatment or as neoadjuvant therapy are intriguing possibilities, he said, as are the development of KRAS-targeted molecular glues and the use of immunotherapy to improve responses.
Closing Keynote Identifies Therapeutic Vulnerabilities in Pancreatic Cancer
After three jam-packed days of innovative ideas, insightful commentary, and lively interactions, the meeting closed with a keynote lecture by AACR Past President David Tuveson, MD, PhD, FAACR.

In his presentation, Tuveson shared findings from mouse models that identified potential new therapeutic targets in RAS-mutated pancreatic cancers. His findings suggest that the NF1/SPRED2/RSK1 membrane-targeted complex may have important roles in regulating the oncogenic activity of KRAS and implicate the cholesterol-modifying enzyme SOAT1 as a potential therapeutic vulnerability.
“The Joy of the Chase”
As a final note to conference attendees, Tuveson spoke of the power of passion and collaboration in driving progress against RAS-driven tumors.
“It’s the joy of the chase,” Tuveson remarked, that motivates him to keep working on this problem. He beseeched all conference attendees to channel their passion to “do what you’re best at to ensure that in five years, we’re looking at durable benefits for our patients.
“I’m hopeful that we will collectively … think of better ways to [target RAS].”
“We’re at a real tipping point here where time actually matters in what we do and how quickly we get these [drugs] to patients,” commented Aguirre. “It is incumbent on all of us to work together … to work with pharmaceutical companies to develop appropriate trials, to share data early and often.”
McCormick echoed these sentiments, drawing parallels between the lab and his other home—the racetrack. Research and racing both rely on teamwork, he noted, and both thrive on an undeniable rush of adrenaline.
The upcoming AACR Annual Meeting 2023 will include a plenary session on targeting RAS, featuring a presentation by McCormick titled “The Race to Kill RAS.” Click here to register.
Learn more about this topic: